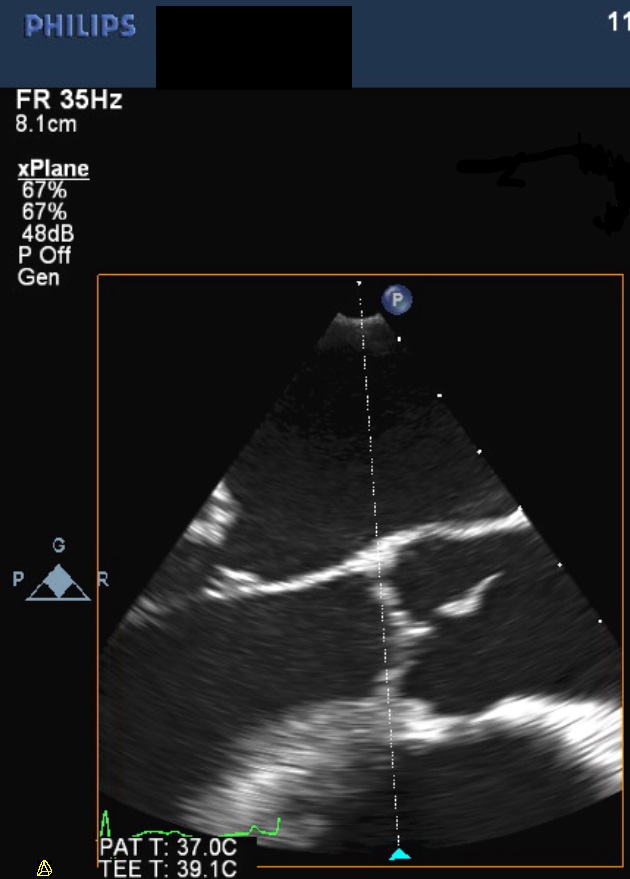
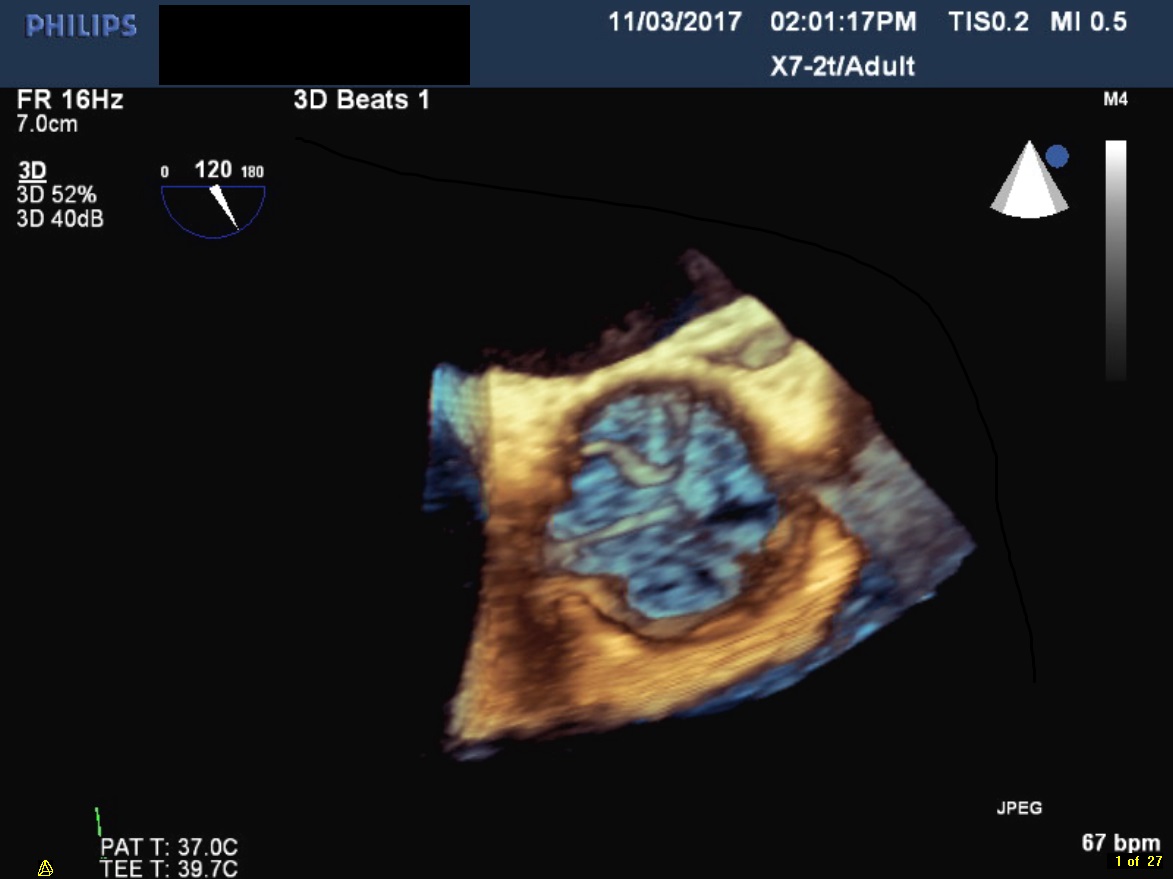
Case Presentation: A 66-year-old female presented to the hospital with two days of acute chest pressure which occurred at rest. It was intermittent in nature but had persisted over the past two days which prompted her to present to the hospital. She had a past medical history of diabetes mellitus, hypertension, and heart failure with a preserved ejection fraction. Her only home medication was furosemide. Vitals were significant for blood pressure in the 180s/80s. Physical examination was normal, without signs of volume overload or decompensated heart failure. Her basic labs including complete blood count and chemistries were unremarkable, however, she was noted to have an elevated troponin at 0.817 ng/mL which eventually peaked that evening at 4.630 ng/mL. Electrocardiograms showed nonspecific ST-segment and T-wave changes. She met criteria for acute coronary syndrome and therefore was started on a heparin drip and dual anti-platelet therapy. A transthoracic echocardiogram was performed which showed a newly-depressed left ventricular ejection fraction to 29%; additionally, a small mobile mass was also noted on the aortic side of the aortic valve. Due to the mass’s proximity to the coronary ostium it was felt that performing coronary angiogram would be high-risk, and so a coronary CT angiography was performed instead. It showed moderate disease without any severe or culprit lesion. Dual anti-platelet therapy was discontinued, the patient was placed on apixaban, and she was discharged with cardiothoracic surgery follow-up for removal of a presumed cardiac papillary fibroelastoma.
Discussion: The majority of myocardial infarctions are caused by coronary atherosclerosis. Occasionally, however, there are other causes such as arterial dissection and coronary vasospasm. This case highlights another rare cause of myocardial infarction caused by a tumor of the aortic valve. Cardiac papillary fibroelastomas (CPF) are the most common primary heart valvular tumor. CPF are known to cause both cerebrovascular accidents, as well as angina and on occasion myocardial infarction. The mechanism of cerebrovascular accident is felt to be embolism, either of tumor-associated thrombus or of tumor fragment itself. Myocardial infarction is felt to be caused by either embolism from the tumor into the coronary arteries, or by direct obstruction of the coronary ostia. In this case coronary CT angiography was used as an alternative to invasive coronary angiography to rule out atherosclerotic coronary disease, as there was a risk of complication with invasive evaluation.
Conclusions: This case highlights an unusual cause of acute coronary syndrome. Given the risks of invasive coronary angiography in this case, coronary CT angiography was used to exclude coronary atherosclerotic disease as the cause of NSTEMI in this patient. We presume that the cause of the patient’s myocardial infarction was the cardiac papillary fibroelastoma, via either embolism from the tumor itself to the coronary arteries or via direct obstruction of a coronary ostia.