Background: Syncope scores San Francisco Syncope Rule (SFSR) and Evaluation of Guidelines in Syncope Study (EGSYS)(1) are used as screening tools for predicting adverse outcomes among patient with syncope(1, 2). Surprisingly for scoring systems used for risk stratification of same clinical condition, differ significantly based on variables of importance used in calculating individual scores. An evaluation of concordance in performance of these two scoring systems in a cohort of geriatric population with predisposition for multi-causation disease model is not reported in literature. We hypothesized concordance of classifying high risk syncope patients will not be perfect since they used different clinical parameter to calculate the scores.
Methods: In this single center retrospective cohort study, we evaluated patients of age 65 or above presented to a large academic center with syncope during the period of 01/01/2017 to 12/31/2018. Patients with confirmed non-syncopal syndromes, active acute medical condition, drug or alcohol use prior to the event were excluded from study. Data on demographics, clinical presentation, laboratory, echocardiogram, treatment and outcome were collected by retrospective chart review in redCap data management system. Data quality was assessed to minimize inter-observer variability using a representative sample from the cohort. At the completion of data collection EGSYS and SFSR scores were calculated and dichotomized as low and high risk patients based on set criteria of the scoring system. Demographic, clinical characteristics and prevalence of adverse events were calculated among EGSYS and SFSR risk categories. Least squared means and likelihood ratio were used to find significant difference across the categories for continuous and categorical variables respectively. Concordance analysis was performed using two by two tables among two scoring methods and kappa co-efficient was calculated. SAS version 9.4 was used for statistical analysis.
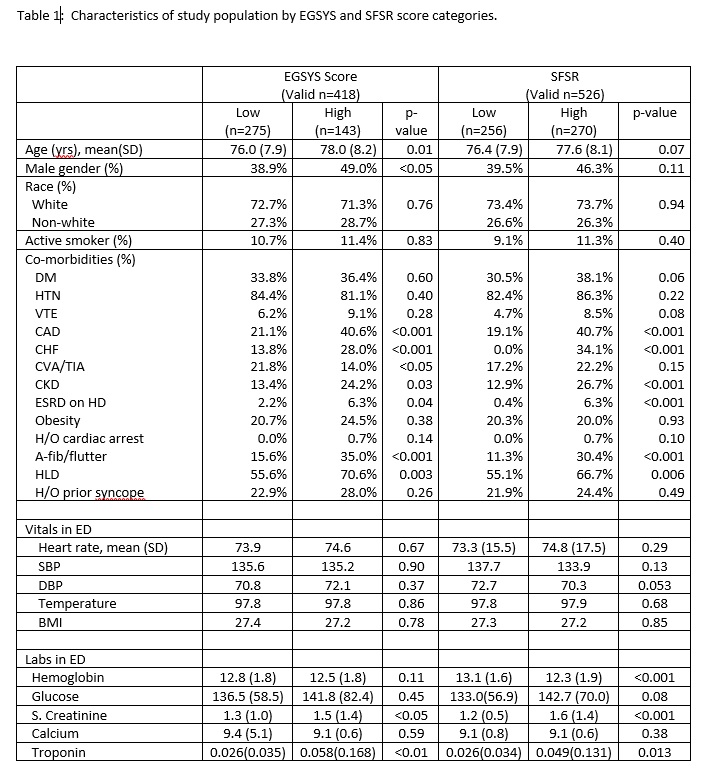
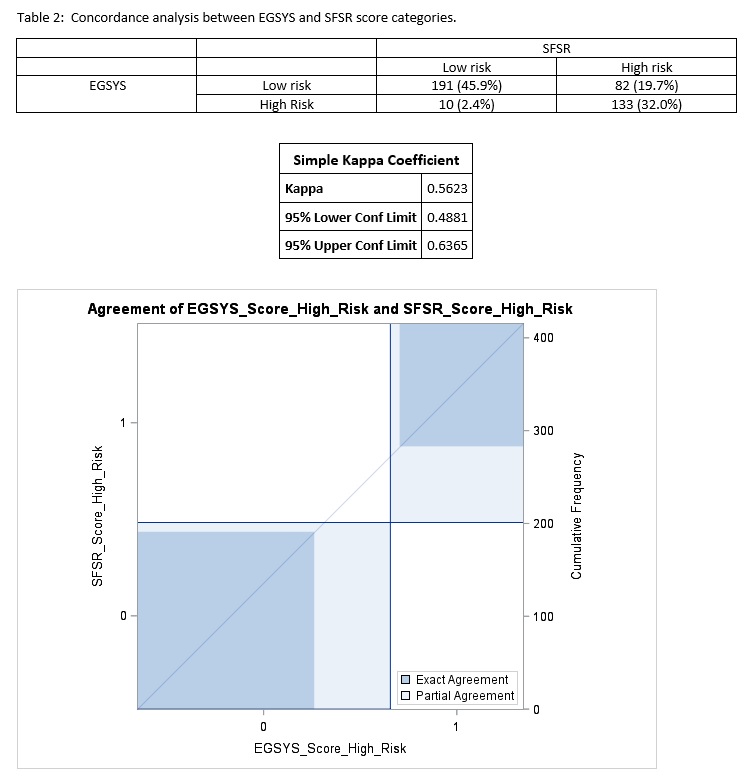
Results: Among 548 eligible study population, EGSYS and SFSR score could be calculated in 418 and 526 patients respectively. Prevalence of high risk EGSYS and SFSR scores were 34.2% and 51.3% respectively. High Risk EGSYS score group was older (mean age 78.0 years) and had male predominance (49%) compared to low EGSYS score group. No such difference was present among SFSR groups. Prevalence of smokers, co-morbidities, emergency department vitals and labs were very comparable with small differences in certain variable among two groups within each system. Statistically non-significant but higher trend of 48 hours adverse outcome were noted in high risk groups. In concordance analysis 45.9% and 32.0% patients were identified as low and high risk, respectively, by EGSYS and SFSR scoring methods. 19.7% patient who fell into high risk group based on SFSR, were grouped as low risk by EGSYS. 2.4% patients were classified as low risk by SFSR but fell in high risk group in EGSYS methods. Kappa coefficient (95% CI) of agreement between the two scoring methods was 0.56 (0.49, 0.64).
Conclusions: In the same geriatric population prevalence of high-risk score was lower using EGSYS method than SFSR method. Strength of agreement is moderate between the two scoring system. Further study is warranted to examine each component of scoring methods and identifying strategies to improve agreement between the methods.