Background: Anemia is a risk factor for cognitive impairment as a result of reduced delivery of oxygen to the brain from low hemoglobin (Hb) levels. In ambulatory patients, mild anemia (Hb 10-12g/dL) has been associated with reductions in patients’ cognitive function [1–3]. In hospitalized patients it is standard of care to maintain Hb levels far lower, between 7-8g/dL, as a result of restrictive transfusion practices [4]. This raises the possibility that the lower Hb levels allowed in hospitalized patients, as a result of restrictive transfusion practices, may have a deleterious effect on patients’ cognitive function. This is important because reduced cognitive function negatively effects patients’ self-efficacy and functioning, which may impair functional status and recovery after hospital discharge. While transfusion trials in hospitalized patients have shown no difference in outcomes between restrictive vs. liberal transfusion thresholds, these RCTs did not examine the effect that lower Hb levels may have on patients’ cognitive function [5]. Thus, it remains unknown whether lower Hb levels during hospitalization may effect cognitive functioning, and to date there is no data describing the effect of lower Hb levels on cognitive function in hospitalized patients with anemia. Therefore, the purpose of this study was to collect data on and test for an association between Hb levels during hospitalization and cognitive fatigability, a measure of cognitive function.
Methods: From 7/2017-2/2019, hospitalized general medicine patients with a Hb <10g/dL were approached for an inpatient interview at hospital admission. Cognitive fatigability was measured using the Pittsburgh Fatigability Scale (PFS) [6], a validated instrument for measuring cognitive fatigue in the context of specific activities of fixed duration. PFS scores range from 0-50, with higher scores indicating greater cognitive fatigability (worse cognition on any given activity). Patients’ Hb values and clinical data were abstracted from hospital administrative databases. Linear regression was used to test the association between cognitive fatigability (PFS) as the dependent variable and patients’ Hb and age as the predictor variables of interest, controlling for race, gender, sickle cell anemia (SC), gastrointestinal bleeding (GIB), dementia, and depression (MDD), since these comorbidities effect both anemia and/or cognitive function.
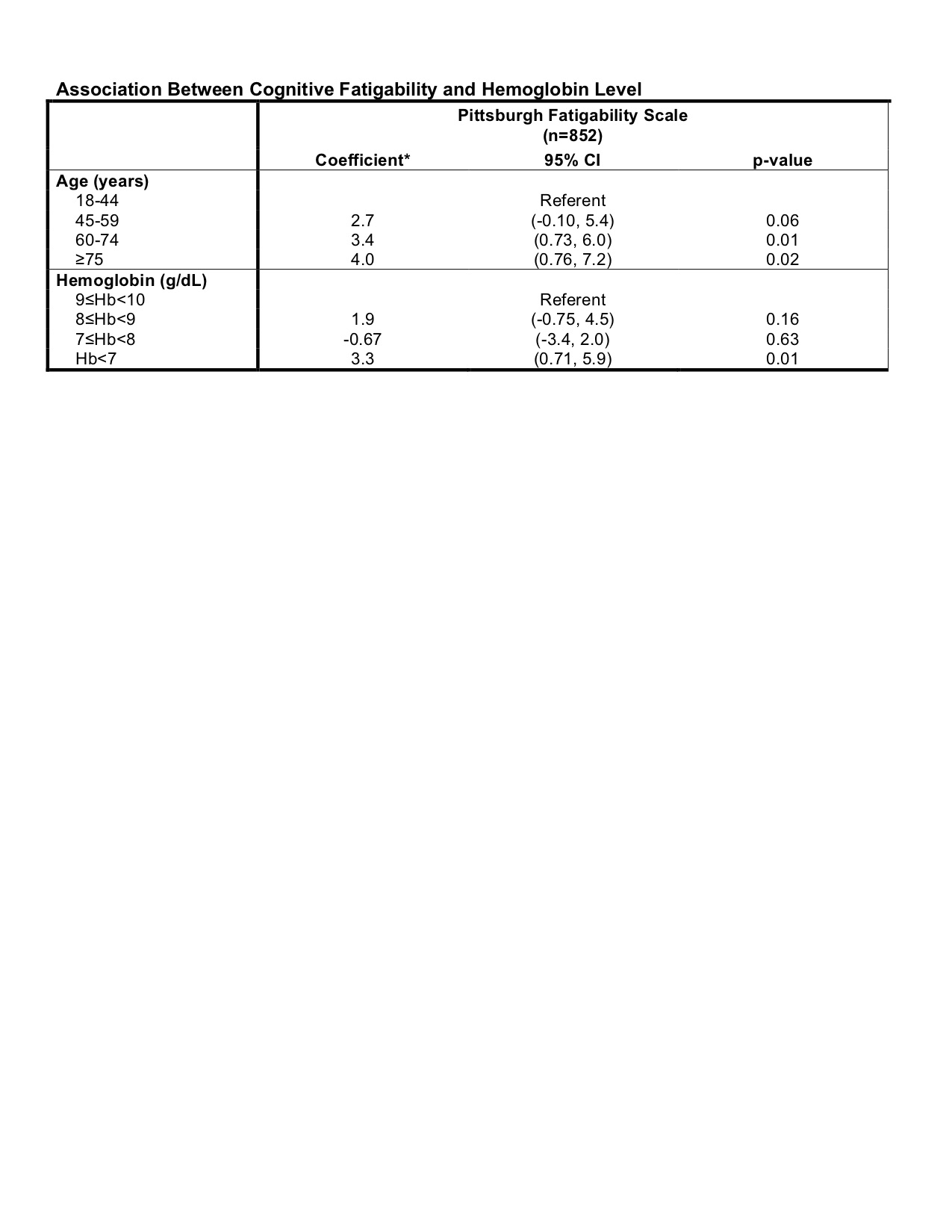
Results: 852 patients completed the inpatient interview. The average age was 58 (±18), 59% were female, 73% were African American. The mean Hb was 8.9g/dL (±1), and the average nadir Hb was 7.9g/dL (±1). Ten percent (10%) of patients had SC, 9% had GIB, 3% had dementia, and 15% had MDD. In the regression model, worse cognitive fatigability (decreased cognition) was associated with and statistically significant in patients with older age (60-74 β=3.4, p=0.01, 75+ β=4.0, p=<0.02), and for patients with a Hb 7g/dL during hospitalization (see table).
Conclusions: In hospitalized patients with anemia, older age and a Hb level below 7g/dL are associated with increased cognitive fatigability and worse cognition, while Hb levels above 7g/dL are not associated with decreases in cognitive fatigability or worse cognition. These findings are in line with and support restrictive transfusion practices, which recommend maintaining patients’ Hb levels between 7-8g/dL, and only transfusing a patient when their Hb drops below 7g/dL.