Background: Heart failure (HF) is a major cause of hospital readmissions and healthcare costs. HF patients have the highest rate of unexpected readmission of all diseases tracked by the Centers for Medicare and Medicaid Services (CMS), at 21.2% (1). HF prevalence is also projected to increase 46% from 2012 to 2030, with total costs rising from $30.7 billion to $69.7 billion by 2030 (2). A readmission also increases the risk of both additional hospitalizations and mortality, particularly within one month of discharge (3). Research into improving care of patients during hospitalization and the first month after discharge could reduce both 30-day HF readmissions and mortality.
Methods: A mixed-methods model incorporating qualitative and quantitative designs was performed. Data was collected on grounded theory using a sample of HF cases at a single hospital for the goal of facility and system quality improvement. The EMRs of all patients readmitted for HF exacerbation within 30 days of a previous HF admission from January through December 2018 were reviewed. From December 2018 through January 2019, all patients admitted with HF were offered to be interviewed by medical students during their hospital stay in an in-depth individual standardized open-ended interview format to learn more about how they understood and managed their HF and the barriers affecting their care.
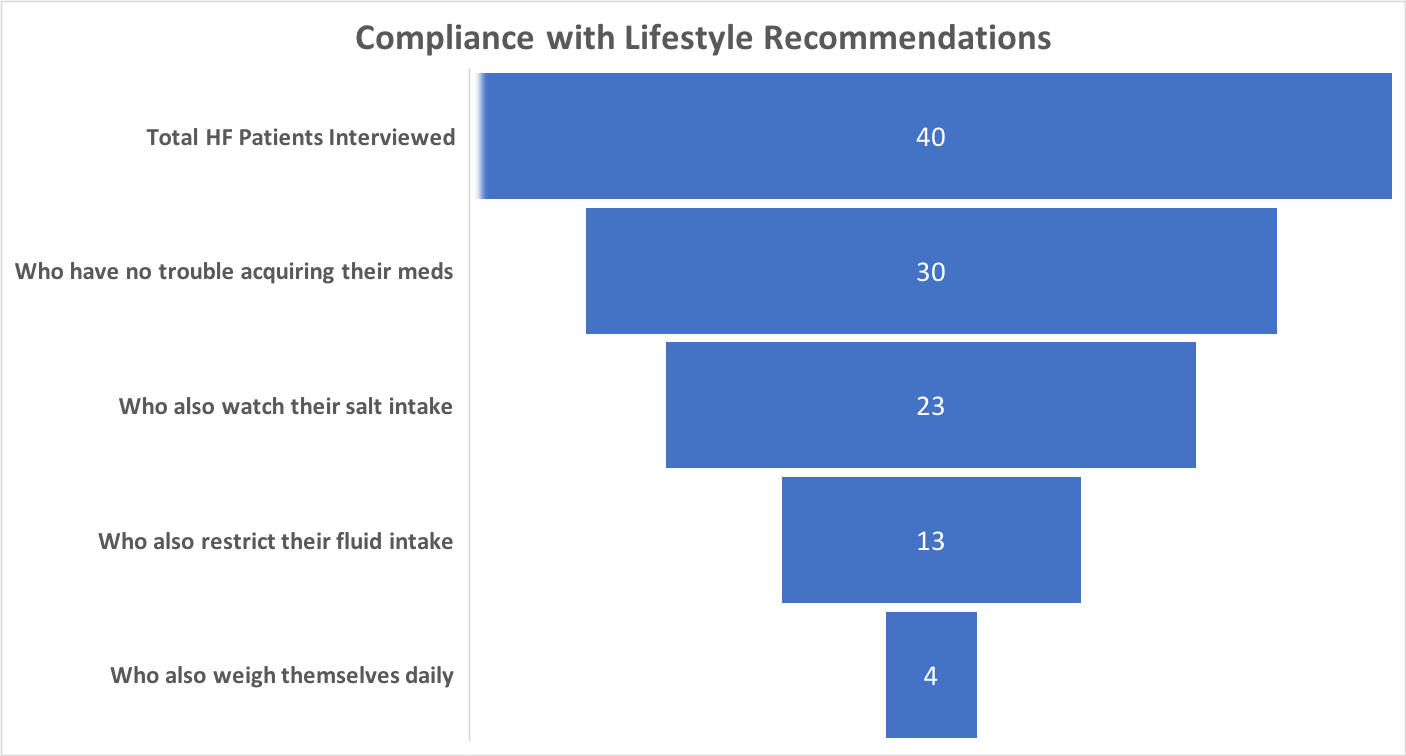
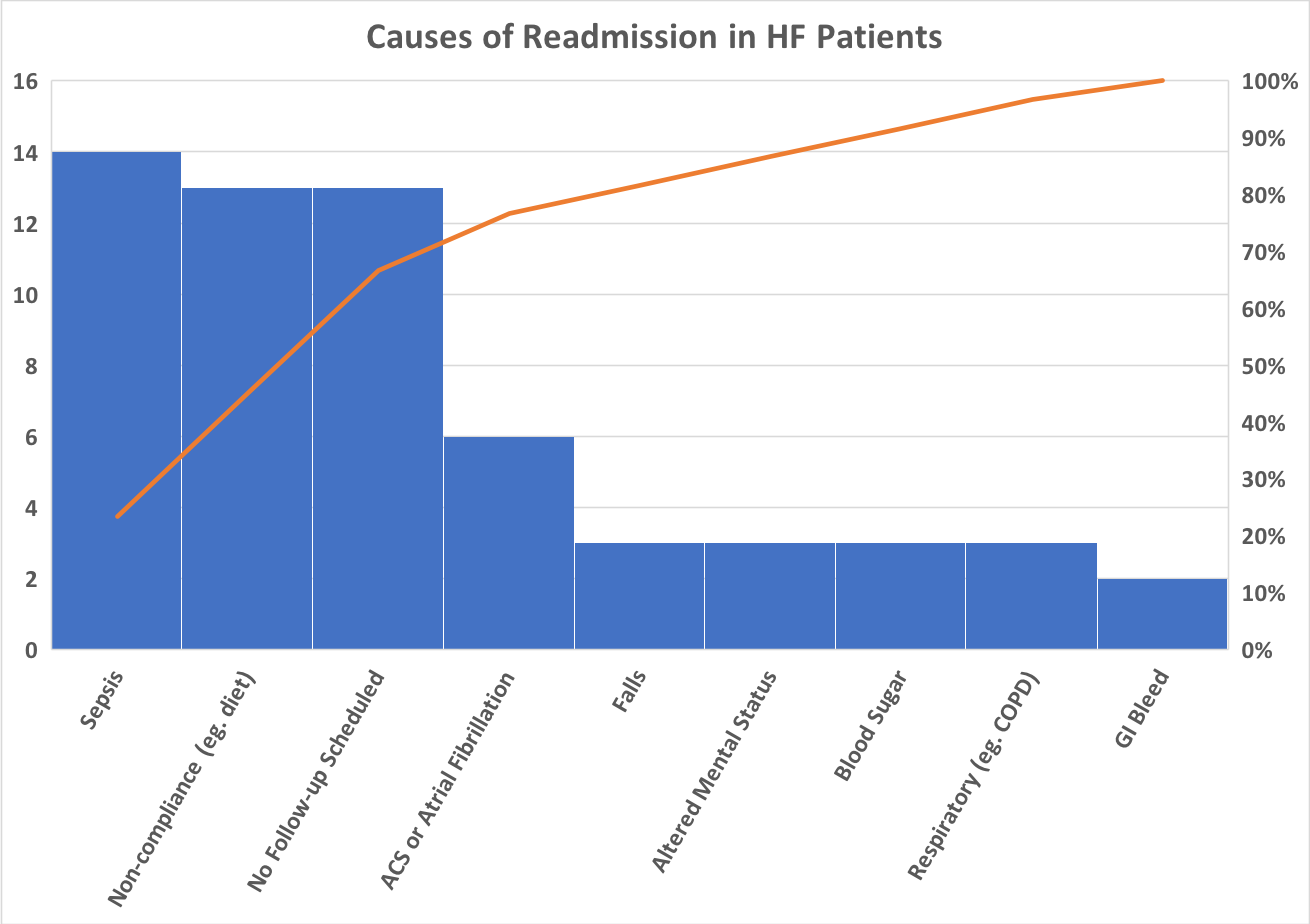
Results: Chart review: There were 80 30-day readmissions for HF. 45% of readmissions occurred within one week of discharge. 47 of patients (59%) received follow-up with the cardiology clinic or their primary care physician within 7 days of discharge. Another 20 patients (25%) received follow-up in 8-30 days, but 13 patients (16%) were not scheduled for a follow-up appointment. 21 of the 80 patients were discharged on the weekend. Of these 21, follow-up appointments within 7 days were not made for 13, or 62% of all HF patients discharged on the weekend. Interview: 40 patients consented to interview. 22.5% of patients reported having run out of their HF medications at least once. 72.5% of patients reported having a scale at home, but only 27.5% reported measuring their weight daily. 25% of patients were not aware of any relation between their diet and HF, 22.5% reported not monitoring the amount of salt in their diet, and 40% reported not following any fluid restriction recommendations. Few patients reported being able to follow their medication and lifestyle recommendations, as depicted below.
Conclusions: Early follow-up has been shown to reduce rates of readmission and mortality (4, 5, 6). In this study, the low rate of early follow-ups for patients discharged on the weekend made it one of the most common factors contributing to readmissions, behind only sepsis, as depicted below. Many outpatient clinics are closed on weekends, so optimizing communication with outpatient clinics throughout the week would close the gap for these patients who require early follow-up appointments. The interview and chart review data showed similar rates of compliance. The interview elicited reasons for noncompliance, including: medication cost, transportation difficulties, underestimating the importance of diet and weight, or not understanding recommendations. Early and regular patient follow up allows for discussion and monitoring of lifestyle changes, optimizing medications, and ensuring access to care. The low rates of patient-reported understanding and compliance with recommendations as well as the high rate of one-week readmission are both areas meriting further study.