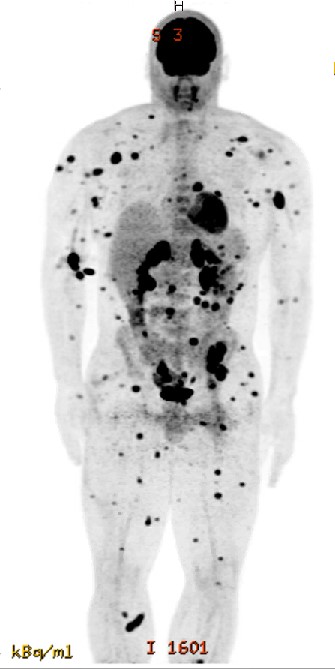
Case Presentation: A 31 yo male bodybuilder with a history (> 10 yrs) of testosterone and aromatase inhibitor (AI) use presented to the ED after a focal seizure. He reported recent difficulty with fine motor function, unintentional weight loss, and growth of multiple painless nodules over the past 3 to 6 months.Physical exam revealed inguinal and supraclavicular LAD; several non-tender nodules over arms, legs, back, abdomen; and numerous nevi over his trunk. Labs were unremarkable except for elevated CK (2622), LDH (322), and mildly elevated AST.Head CT showed a left frontal mass concerning for metastasis. Subsequent brain MRI revealed multiple metastatic lesions and parietal lobe mass with hemorrhagic conversion. Abdominal CT showed a pelvic mass concerning for rhabdomyosarcoma. PET CT demonstrated innumerable hypermetabolic subcutaneous and intramuscular lesions; nodal, visceral, osseous mets; no primary malignancy was identified. Pathology from an abdominal wall subcutaneous nodule was consistent with cutaneous melanoma. Radiation Oncology was consulted, and urgent stereotactic radiosurgery followed by immunotherapy was scheduled. He was discharged on levetiracetam and advised to stop using testosterone, given the concern that it may contribute to progression of disease.
Discussion: Hospitalists may not know that melanoma is more common and much more deadly in men, and skin exams are often under-emphasized. Male vs. female incidence is 27.4 vs. 16.8 per 100,000; male vs. female mortality is 3.9 vs. 1.6 per 100,000. (1) “[F]emales retain a 38% survival advantage compared to males after adjusting for stage at diagnosis…have thinner tumors, less tumor ulceration, less progression to lymph node or organ metastases, longer delay before relapse, and a higher cure rate.” (1)Although there have been no clinical trials examining sex hormone modulation in treatment of melanoma, some studies have shown that “high androgen levels can directly stimulate melanoma cell proliferation and tumor growth in a dose-dependent manner.” (2) Research suggests that “estrogens are directly and indirectly inhibitory for melanoma tumorigenesis while androgens can directly promote melanoma tumorigenesis and indirectly inhibit melanoma immunotherapy.” (2) Androgen receptors (AR) increase melanoma invasion by upregulating the matrix metalloproteinase MMP9. (3) AR, along with EGR1, also binds to long non-coding RNA SLNCR; this triad represses tumor suppressor p21, leading to further tumor proliferation and invasion, which could help explain why men have higher incidence, and more rapid progression, of melanoma. (4)
Conclusions: The role of testosterone in predisposing to, or fueling the progression of, melanoma remains unclear. However, available evidence suggests that exogenous testosterone could play a yet-as-unidentified role in melanoma tumorigenesis and lead to worse outcomes. Our patient injected testosterone and took AIs for years, which may have contributed to his widely metastatic presentation, and we present this case to raise the possibility of, and heighten observation for, other similar cases. Asking about testosterone use, in addition to history and thorough skin examination, may be helpful in assessing risk for melanoma.Given the likelihood men will have more rapid progression, earlier metastases, worse treatment response, and worse prognosis, hospitalists should be vigilant for possible melanoma, especially in men presenting with metastatic disease of unknown primary.