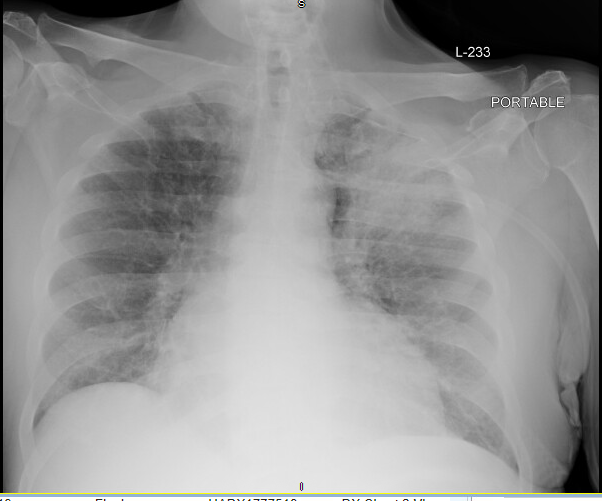
Case Presentation: The patient is a 60-year-old male with chronic mixed systolic and diastolic heart failure, Chronic Obstructive Pulmonary Disease (COPD), and Obstructive Sleep Apnea (OSA) who was admitted to general medicine due to a 4-week history of progressive dyspnea and lower extremity edema, concerning for a heart failure exacerbation. Eight days into his hospital course, the patient developed worsening dyspnea, tachypnea and a productive cough with bloody sputum. On exam, he was febrile to 102F; his neurologic and psychiatric exams were notable for hypervigilance, and visual hallucinations concerning for delirium. Labs were notable for a WBC to 15.36 with a neutrophilic predominance and hyponatremia with a serum sodium of 120mmol/L. Chest X-ray was notable for an increasing left apical hazy opacity consistent with left upper lobe pneumonia. Blood cultures were drawn and patient was started on empiric antibiotic therapy with Vancomycin and Cefepime. Over the subsequent 5 days, the patient continued to decline with worsening hyperactive delirium and paranoid delusions despite broad spectrum antibiotics. In addition, he developed acute kidney injury with peak BUN and creatinine of 119 and 8.3, respectively. On hospital day 15 a urine antigen test for legionella resulted positive, and he was started on a 10-day course of levofloxacin. Over the subsequent week, his encephalopathy, renal failure, hyponatremia and leukocytosis all resolved. Infection control in the hospital investigated and determined this to be a case of hospital acquired legionella infection.
Discussion: Hospital acquired legionella infections make up 4-8% of all legionella pneumonia cases and carry a mortality rate of up to 30-50%, due in part to delayed diagnosis and treatment. Infection with legionella pneumonia is most commonly acquired as a result of inhalation of aerosolized water droplets from contaminated aerosolized water sources and is associated with a rapidly progressive pneumonia with severe extrapulmonary manifestations including encephalopathy, renal failure, and hyponatremia. Risk factors for this infection include male gender, cigarette smoking, and poorly managed comorbid health conditions. Per 2019 Infectious Disease Society of America (IDSA) guidelines for Community Acquired Pneumonia (CAP), patients who meet criteria for severe infection should have urine and sputum legionella testing as part of their diagnostic workup. Of note, despite the high mortality rate associated with hospital acquired legionella pneumonia, this clinical entity is not mentioned in 2016 IDSA guidelines for Hospital Acquired Pneumonia (HAP). This omission may contribute to delay in recognition of this pathogen by hospitalists when patients develop a syndrome consistent with HAP. In this case of hospital acquired pneumonia complicated by delirium, renal failure, and hyponatremia, early clinical suspicion for legionella infection may have led to an expedited diagnosis.
Conclusions: Due to the high mortality associated with legionella infection, it should be considered on the differential diagnosis for hospital acquired pneumonia, especially if there are atypical or extrapulmonary manifestations. In these cases, urine and sputum legionella testing should be sent.