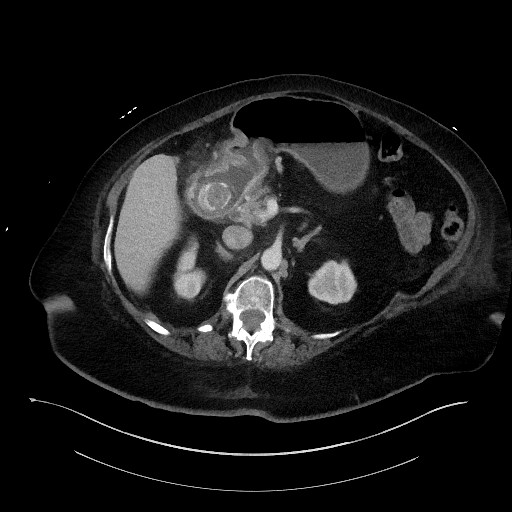
Case Presentation: 79 yo. female with PMH of A. Fib on Warfarin, HFpEF, Hypertension,PVD, CKD-III who presented to the hospital with generalized weakness and recent falls. Reported gradual decline over about 1 month before admission. She reported that symptoms started with “stomach flu” about 4 days prior with chills, nausea, and abdominal pain. She complained that for about 1 week she had not been able to eat anything due to nausea and emesis. She described the emesis as nonbilious, sometimes brown, and usually whenever she just tried to eat, pain was waxing and waning in severity, and located across her mid-abdomen, KUB normal. PE:Abdomen: Soft. Bowel sounds hypoactive. Tenderness on palpation over the epigastric region with no guarding, rebound tenderness or rigidity. Labs notable for Hypokalemia, normal LFT’s, normal CXR. A CT scan showed a gastric obstruction related to gallstone with a cholecystoduodenal fistula with a large gallstone within the duodenal bulb. Patient was conservatively managed by NPO, NG tube placement, empiric antibiotics for coverage of biliary and upper GI organisms given the degree of her symptoms of an obstructive process, Upper GI endoscopy showed a large obstructing gallstone measuring about 4-5cm in the duodenal bulb associated with duodenal ulcer. Cholecystoduodenal fistulous tract was seen in the bulb/first portion of the duodenum.
Discussion: Various modalities are used to make the diagnosis once the condition is suspected clinically. Management choices include ERCP, lithotripsy and surgery. Prognosis related to early recognition, management of comorbid conditions, and careful selection of treatment modalities. Imaging was consistent with Bouveret’s syndrome, a rare form of gallstone ileus in which a cholecystoenteric fistula leads to an impacted gallstone in the duodenum and subsequent gastric outlet obstruction. Bouveret’s syndrome is a rare variant of gallstone ileus, caused by the impaction of gallstone in duodenum. The gallstone erodes through the wall of gallbladder and duodenum creating a bilioenteric fistula due to persistent inflammation in the surrounding area and pressure necrosis.Gallstone ileus causes intestinal obstruction in 1%-4 % of the cases, of which Bouveret’s syndrome comprises of only 1%-3%. It is more common in women ,median age of 74 years. This clinical entity owing to proximal gastrointestinal obstruction, usually caused by large (usually >2.5cm) gallstone. Clinical presentation can vary from gastric outlet obstruction as seen in our case, to acute pancreatitis, upper gastrointestinal bleeding, duodenal perforation, Boerhaave’s syndrome, gastric bezoars formation. A classic Rigler’s triad of dilated stomach, pneumobilia, and ectopic stone appearing as a filling defect in the duodenum seen on a CT scan is virtually pathognomonic of the Bouveret’s syndrome. This is diagnostic in only 21% of the cases with a conventional radiograph. High clinical suspicion with appropriate diagnostic imaging helps make the diagnosis easier.
Conclusions: Bouveret’s syndrome is rare and remains a diagnostic and therapeutic challenge. CT scan is the diagnostic method in 60% of cases. Various endoscopic or percutaneous methods have been described for treatment (mechanical, laser, intra/extracorporeal electrohydraulic lithotripsy). Although surgery remains the first treatment option and 91% of patients will need surgery during the disease. Hospitalists need to consider Bouveret’s Syndrome in patients with gastric outlet obstruction with CT scan findings.