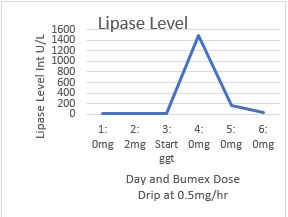
Case Presentation: The case begins with a 71-year-old female named MB. She initially presented with two weeks of worsening back pain, falls, and renal insufficiency. The pain itself radiated from her mid epigastrium to her back. The patient had a past medical history of COPD, paroxysmal atrial fibrillation, and heart failure with reduced ejection fraction. At home the patient was on Eliquis, ProAir, Stiolto, Tylenol, Amiodarone, Benazepril, and bumetanide. Upon presentation to the ED the patient’s vitals were stable with a temperature of 97.6 degrees Fahrenheit, blood pressure 107/59, heart rate 91, and saturating 92% on room air. Labs were pertinent for a BUN 33 and Creatinine 2.2. A complete metabolic panel was obtained on initial presentation with normal transaminase and lipase (11 intU/L). The initial evaluation included an abdominal CT which demonstrated a small 2mm left ureteral stone that was minimally obstructive. On echo the patient’s ejection fraction was determined to be 34% with grade III LV diastolic dysfunction. Prior echo two years earlier demonstrated a left ventricular ejection fraction of 42%. It was felt that the patient’s fluid overload was contributing to her unsteadiness, thus Cardiology was asked to evaluate the patient. Cardiology placed the patient on a Bumex drip on day 3 of hospitalization. One day later the patient began to suffer increasing epigastric and back pain. Two days after starting the drip the lipase was checked due to a suspicion of pancreatitis. Lipase had climbed to 1,487. The medical team diagnosed MB with pancreatitis. It was suspected to be secondary to Bumex, and the drip was discontinued. The symptoms quickly resolved after the discontinuation of the Bumex drip. In fact, lipase levels fell to 43 two days later.
Discussion: Pancreatitis has been reported with the use of diuretics, especially furosemide and thiazides. Hyperamylasemia can also occur in the setting of renal insufficiency due to decreased clearance. The clear relationship between increasing the bumetanide dosage and the clinical presentation of pancreatitis provides strong evidence that the patient’s pancreatitis was likely caused by bumetanide. This is supported by laboratory and clinical findings. Although the mechanism is unclear, possible mechanisms include a direct toxic stimulation of the pancreas causing increased secretion. An alternative hypothesis is that diuretics in general cause extra cellular volume contraction leading to an ischemic insult of the pancreas (Stenvinkel, 1988). However, if that were the case, one would expect a higher prevalence of pancreatitis in patients treated with bumetanide. More studies are needed in order to uncover the underlying cause.
Conclusions: As diuretics are used widely and bumetanide use has been on the rise, it is important to consider diuretics as a cause of pancreatitis in patients. It may be reasonable to consider holding these agents in those whom pancreatitis cannot be explained.