Background: Care of the pediatric patient does not end after the family exits the hospital doors. Post-discharge issues can lead to significant consternation for families, unnecessary risk to the patient, and re-utilization of healthcare resources. Despite careful preparation for transfer of care to the primary care physician (PCP), some post-discharge issues are unanticipated and lead to sub-optimal care. The goal of this work was to improve this transition by including pediatric hospital medicine (PHM) provider contact information on after visit summaries (AVS) as a “safety net” for when families cannot reach their PCP after discharge.
Methods: This is a single center prospective study performed at our freestanding pediatric, 300 bed, quaternary care hospital in the Midwest. In April 2019, PHM team contact information was added to the AVS. This study was approved by our IRB as non-human subjects research.Contact information was automatically built into the PHM AVS, and to promote the PCP-patient relationship, PCP contact information was placed above PHM information. Nursing education was provided to align discharge teaching with the new AVS. Hospital operator education was done to standardize scripting of pages to PHM providers, allowing for expedited chart review prior to returning the call. Feedback sessions were held with PHM providers to discuss balancing safe patient care while not infringing on the PCP-patient relationship. We collected data over a 13-month period with addition of call specific questions to the provider post-shift survey. As a means of quality assurance, a query report in the EHR was run for all call documentation by PHM providers. Descriptive statistics and Fisher’s exact test were used to analyze data.
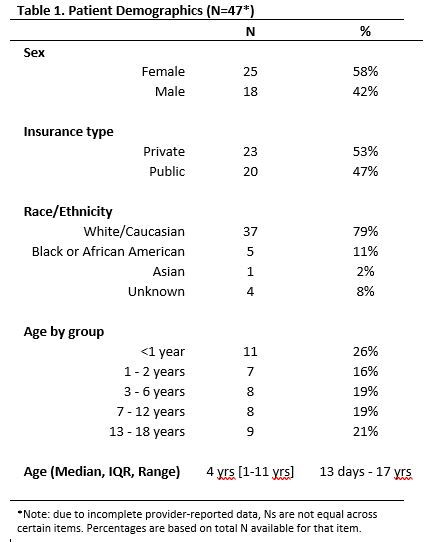
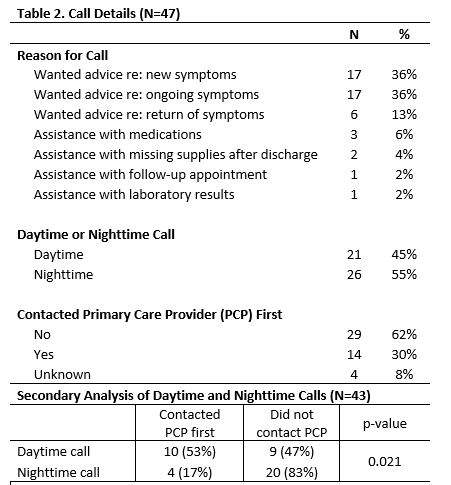
Results: Out of the 5,145 discharges over 13 months, there were a total of 47 calls (0.9% of discharges) from families, averaging 3.6 calls per month. The average length of time spent on a call was 21 minutes. Only 30% of families had tried contacting their PCP first and 55% of calls occurred during the night shift (1730-0730). There was a significant difference in whether caller contacted PCP first between night and daytime (17% vs 53% respectively, p=0.021). The most common reasons for calls were wanting advice about new or ongoing symptoms. Real time problem solving with families included assessing the need for re-evaluation, strategies for medication administration, re-assurance about timeline of recovery, and provision of additional resources.
Conclusions: Although inpatient teams work hard to prepare families for discharge, this study highlights the need for provision of additional support. This work demonstrates a simple intervention to help families when they encounter issues, especially during nighttime hours. With only 3.6 calls per month, this “safety net” is an opportunity for improved care transition without a significant time burden placed on individual providers. Limitations of this study include reliance on provider documentation of calls which may underestimate our numbers, and small sample size limiting our ability to assess impact of our intervention. Our future work will include ongoing call tracking to identify themes and specific transition gaps. A “safety net” for families can help augment care as patients transition to outpatient care. PHM providers can triage issues in real time with families, including filling a need after-hours, and can provide active problem solving through counseling and assessing the need for re-evaluation.