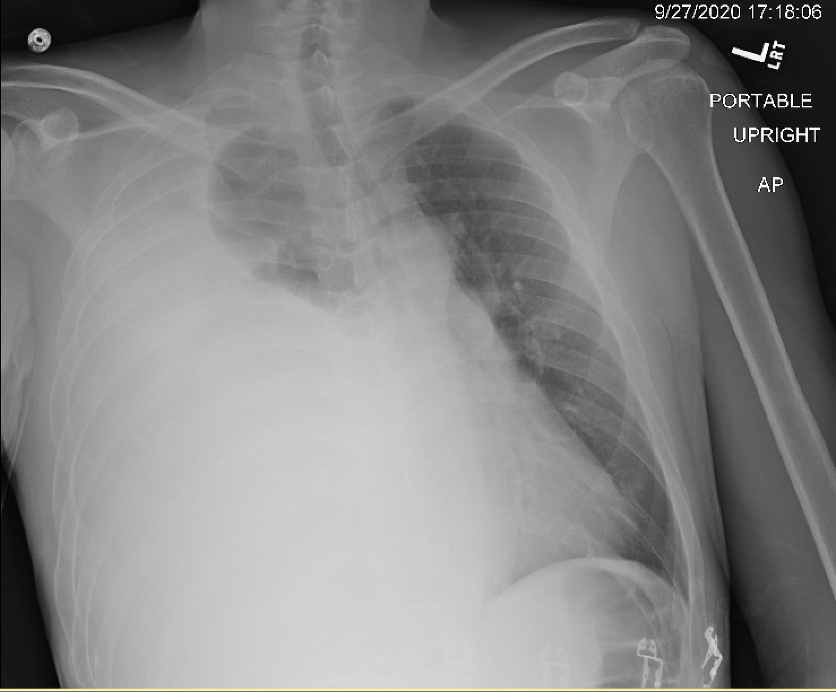
Case Presentation: A 41-year-old male with a past medical history of chronic alcoholic pancreatitis and right-sided pancreatic pseudocyst presented with shortness of breath and right-sided chest pain that began three days prior. Chest X-ray showed near-complete opacification of the right hemithorax. A diagnostic thoracentesis revealed an exudative pleural effusion with a pleural amylase level of 6554 U/L. A chest tube was placed with 3820 mL of serosanguinous fluid output. The patient’s shortness of breath greatly improved. Gastroenterology was consulted who performed Endoscopic Retrograde Cholangiopancreatography (ERCP) which showed a normal ampulla of Vater, but contrast filling of the common bile duct and pancreatic duct showed a disruption of the pancreatic duct with leaking beyond the genu. A sphincterotomy was performed and a double flanged stent was placed. ERCP findings were concerning for pancreaticopleural fistula. Patient’s chest tube had decreased output throughout the hospital stay and daily chest x rays showed stable effusion. Chest tube was removed on the fifth day of hospitalization. The patient was discharged home in stable condition.
Discussion: Pancreaticopleural fistula (PPF) has been recognized as a rare complication of chronic pancreatitis since case reports were published in the 1960s. PPF development is usually due to a leak from an incompletely formed or ruptured pseudocyst, or in a minority of cases due to pancreatic duct leak. Leakage of pancreatic enzymes causes disruption of the fascial layers, forming a fistulous tract between the pancreases the pleura of the lung. This complication most commonly occurs in middle-aged men between 40 and 50 years old who have a history of chronic alcoholism and pancreatitis. In our case, our patient is a middle-aged male with a history of chronic alcohol abuse, chronic pancreatitis, and known pseudocyst which all are known risk factors for PPF formation. Trauma is another cause of PPF but is less common, only accounting for 0.5% of the cases. Clinical manifestations of PPF are usually associated with symptoms of pleural effusions such as dyspnea, chest pain, cough, fever, and septicemia with dyspnea. Pulmonary symptoms are more common than abdominal symptoms, but some patients may primarily complain of abdominal pain consistent with acute pancreatitis. Most pleural effusions are predominantly left-sided; however, right-sided effusions occur in 19% of patients, seen in our patient. The differential diagnosis for pleural effusions is broad so it is important to correlate the patient’s symptoms with their past medical history, lab findings, and imaging to narrow the differential. Pleural effusions secondary to PPF are exudative and amylase levels greater than 1000 U/dL, high pleural lipase, or albumin (greater than 3 g/dL). The diagnosis can be confirmed with ERCP or MRCP. Treatment includes medical management with a chest tube, endoscopic pancreatic duct stent placement, or surgically depending on the patient’s characteristics and the severity of the pleural effusion.
Conclusions: Pancreaticopleural fistula is a difficult diagnosis to achieve and treat at times. Clinicians should have a high suspicion, particularly in the setting of recurrent pleural effusion with a history of pancreatitis and alcohol abuse. Initially, analysis of the pleural fluid amylase will avoid delay in the diagnosis. Subsequently, other options should be considered such as ERCP plus stenting of the pancreatic duct to prevent significant morbidity and mortality.