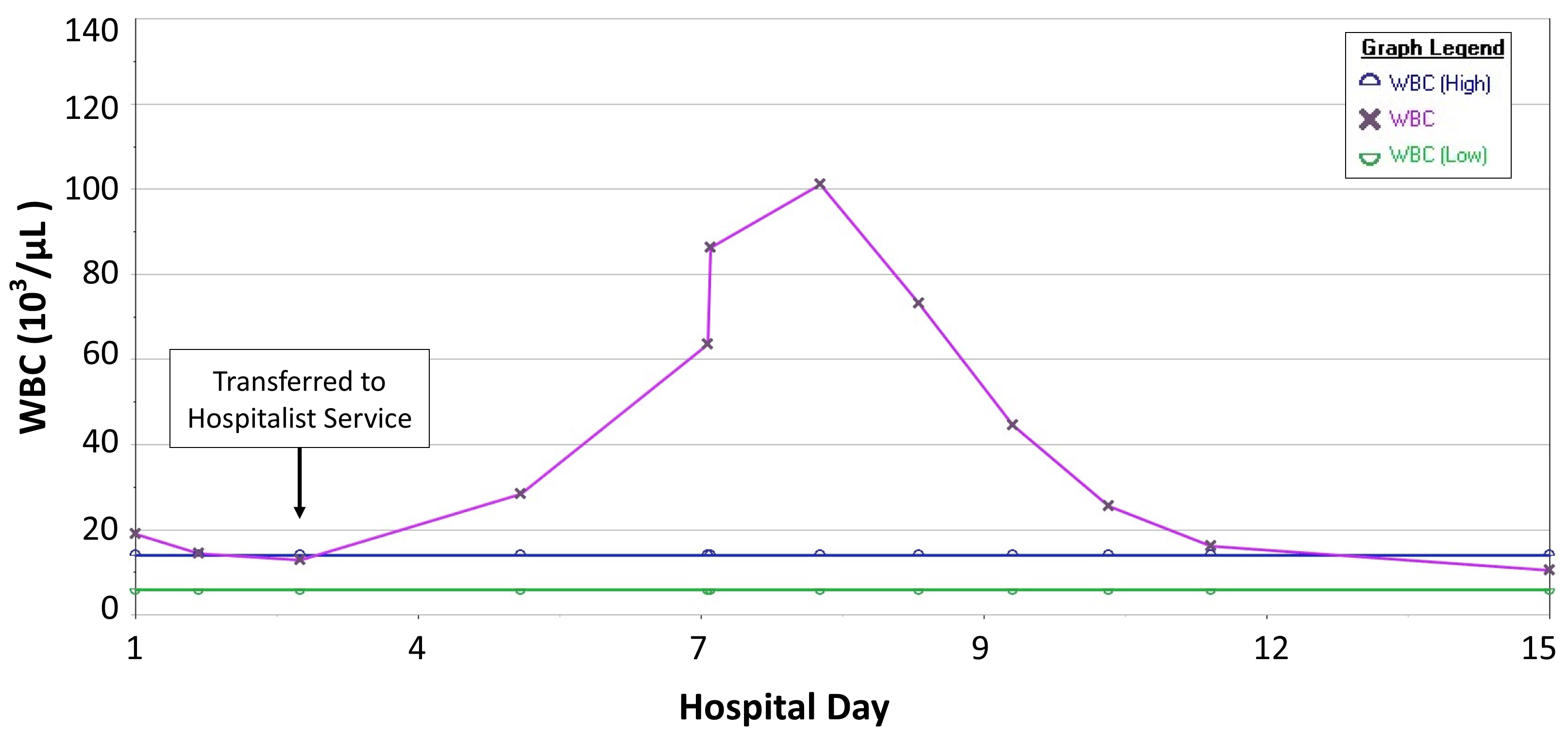
Case Presentation: Previously healthy 2-month-old female presented with 4 day history of fever, rhinorrhea, cough, emesis, diarrhea, decreased intake and progressing rash on abdomen and extremities. Exam notable for injected conjunctiva and flash capillary refill. Patient was admitted to the Pediatric Intensive Care Unit (PICU) for fluid resuscitation and severity of presentation. Given concern for septic shock or toxin-mediated disease, workup included respiratory viral panel (RVP), blood and urine cultures, complete blood count (CBC) and inflammatory markers, and she was empirically started on ceftriaxone. Studies notable for rhinovirus from RVP, elevated CRP (8.4), ESR (26), and Procalcitonin (2.92), and white blood count (WBC) of 19. Cultures showed no growth and vancomycin and clindamycin were added for persistent fevers and poor clinical appearance to mediate potential toxin-mediated disease. Echocardiogram was completed to assess for sequelae of Kawasaki disease (KD) given exam and lab values and found ectatic left coronary artery. Rheumatology was consulted, and she was started on IVIG and methylprednisolone. Labs remained notable for rising ESR to >100 attributed to IVIG and leukocytosis to 20. With clinical improvement, patient was transferred to acute care. She received a second dose of IVIG and steroids due to persistent fevers. WBC continued to rise to a max of 101 (Figure 1). With additional thrombocytosis and anemia on CBC, hematology and oncology were consulted for further assessment of other etiologies of leukemoid reaction. Peripheral smear showed no blasts, and fibrinogen, ferritin, and LDH were normal, reassuring specialists against leukemia, hemophagocytic lymphohistiocytosis, or other bone marrow related processes; specialists agreed that leukemoid reaction was likely due to combination of over-productive/ reactive marrow in inflammatory state with steroid-related demarginalization. Patient remained clinically well appearing as WBC fell from peak and inflammatory markers normalized. She was discharged to home on steroid taper and low dose aspirin with follow up echocardiogram. Outpatient, it was noted WBC and coronary artery changes normalized.
Discussion: Leukemoid reactions in KD are rarely reported in the literature, and there is limited discussion of what degree to expect. In the setting of KD, this is reported more frequently in infants and can be accompanied by other cell-line changes that create concern for oncologic processes. Leukemoid reactions may be indicative of other confounding factors such as infection or oncologic process, or be secondary to IVIG dosing. These factors may lead to complex workup to rule out a broad but concerning differential. In our patient, leukemoid reaction self-resolved with treatment of KD, requiring no further treatment or follow-up.
Conclusions: Leukemoid reactions can occur secondary to KD and may occur to higher levels than expected, possibly due to very reactive bone marrow. While considering serious infections, oncologic processes, or other medical emergencies in infants, KD should also be in the differential diagnosis of such a reaction. An evaluation for other diagnoses may be warranted given patient’s age and mortality risk, but physicians should be reassured if other workup is negative that KD is a potential etiology that requires little intervention outside of previously planned lab follow up and attention to other sequelae.