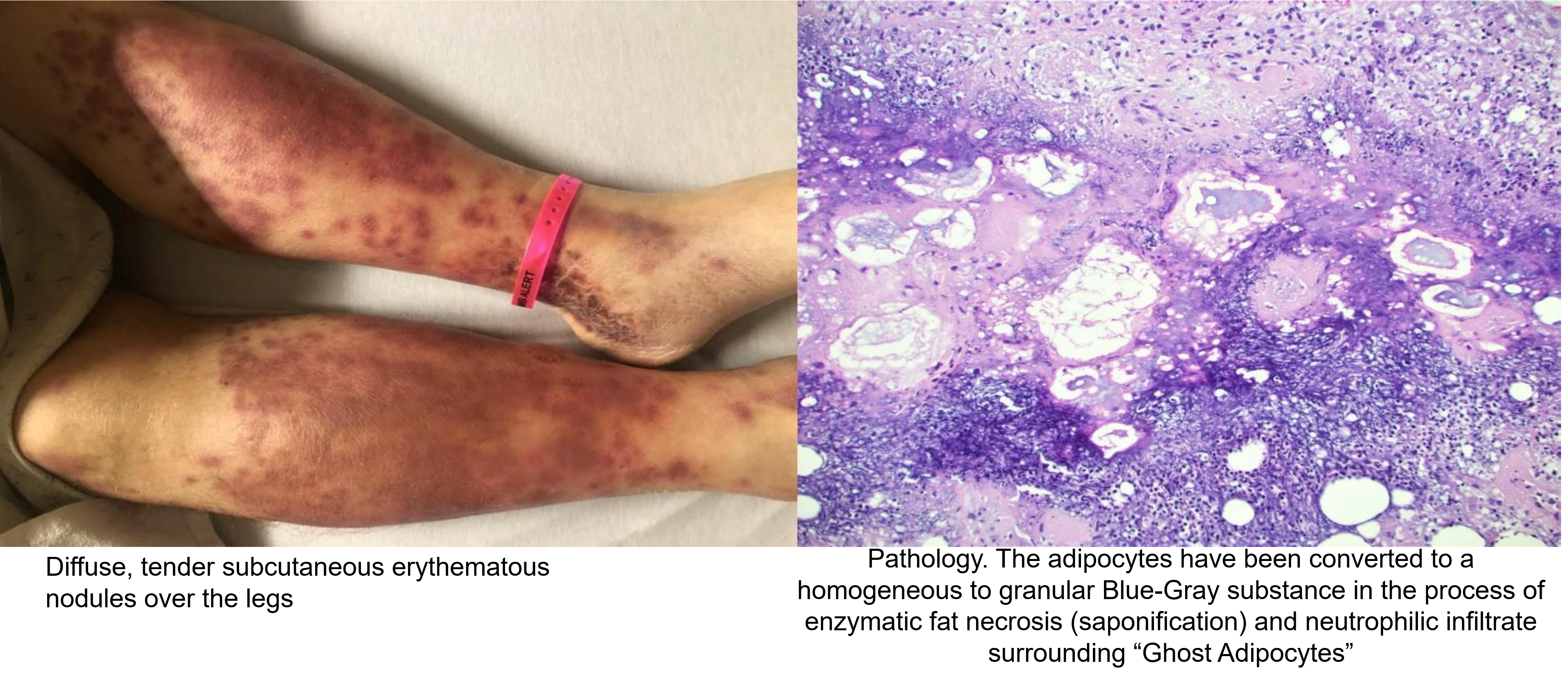
Case Presentation: A 68-year-old male patient with past history of acute pancreatitis, portal vein thrombosis, left lower extremity deep vein thrombosis presented to the hospital with epigastric abdominal pain. His white cell counts were 29,000/ cu.mm and his serum lipase levels was 35,000 U/L. Computed tomography imaging revealed acute necrotizing pancreatitis complicated by pseudocyst formation. Percutaneous catheter drainage of the pseudocyst was done. Later the patient underwent exploratory laparotomy with pancreatic debridement, cholecystectomy, repair of duodenal perforation with an omental patch, and gastric exploration with gastrotomy. During his stay in the hospital, the patient developed bilateral lower extremity swelling and rashes. Physical examination revealed diffuse, painful erythematous nodules over both lower limbs, extending up to his knees. A punch biopsy was performed, and histopathological examination showed lobular panniculitis. He received supportive local wound care for his skin lesions. The skin eruptions disappeared gradually with the resolution of pancreatic inflammation.
Discussion: The diagnosis of pancreatic panniculitis is suggested by the presence of pancreatic disease and pathognomonic histopathological findings onskin biopsy. Biopsy reveals lobular panniculitis without vasculitis. Lesions are characterized by the presence of a predominantly neutrophilic infiltrate surrounding “ghost adipocytes,” which are necrotic fat cells with no nuclei and basophilic granular. cytoplasm, due to calcification.[1,3] Treatment is usually supportive and directed at correcting the underlying pancreatic disease, with lesions resolving once the pancreatic inflammation subsides.[1]
Conclusions: Pancreatic panniculitis is a rare cutaneous complication of an underlying pancreatic disease. Many patients develop skin nodules even before the underlying pancreatic disease has been diagnosed.[1] Therefore, physicians should keep a low threshold for clinical suspicion in such patients and undertake investigations to look for significant underlying pancreatic pathology.