Background: Acute heart failure (AHF) exacerbations are a leading cause of hospitalization in the United States. Despite the frequency of AHF hospitalizations, there are inadequate data or practice guidelines on how quickly diuresis should be achieved.
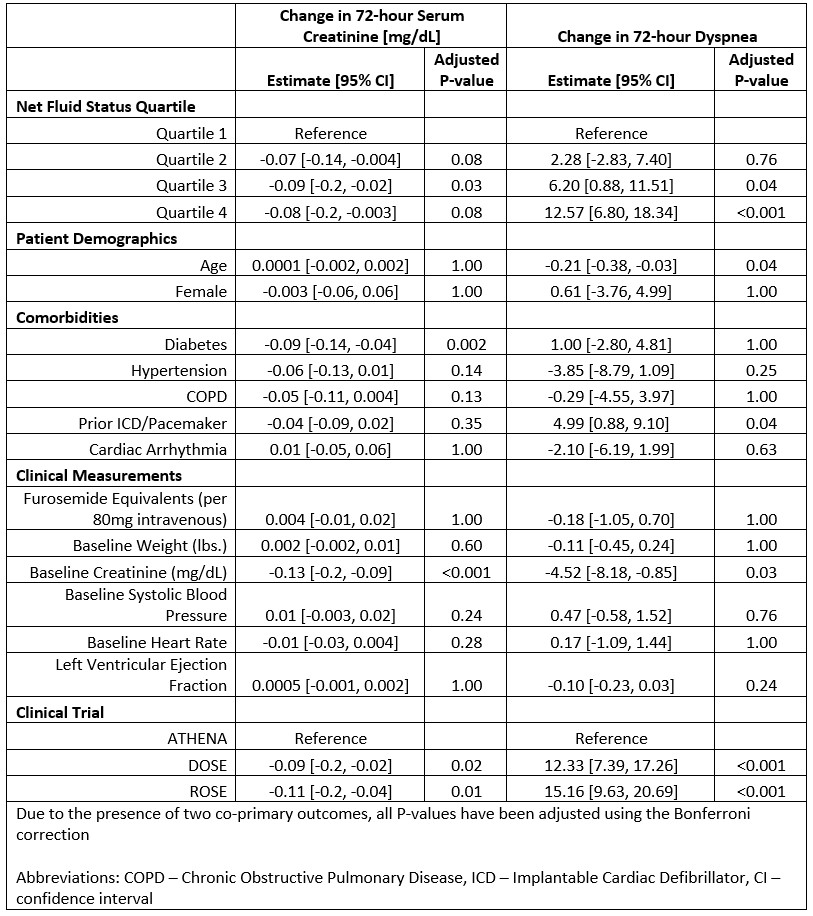
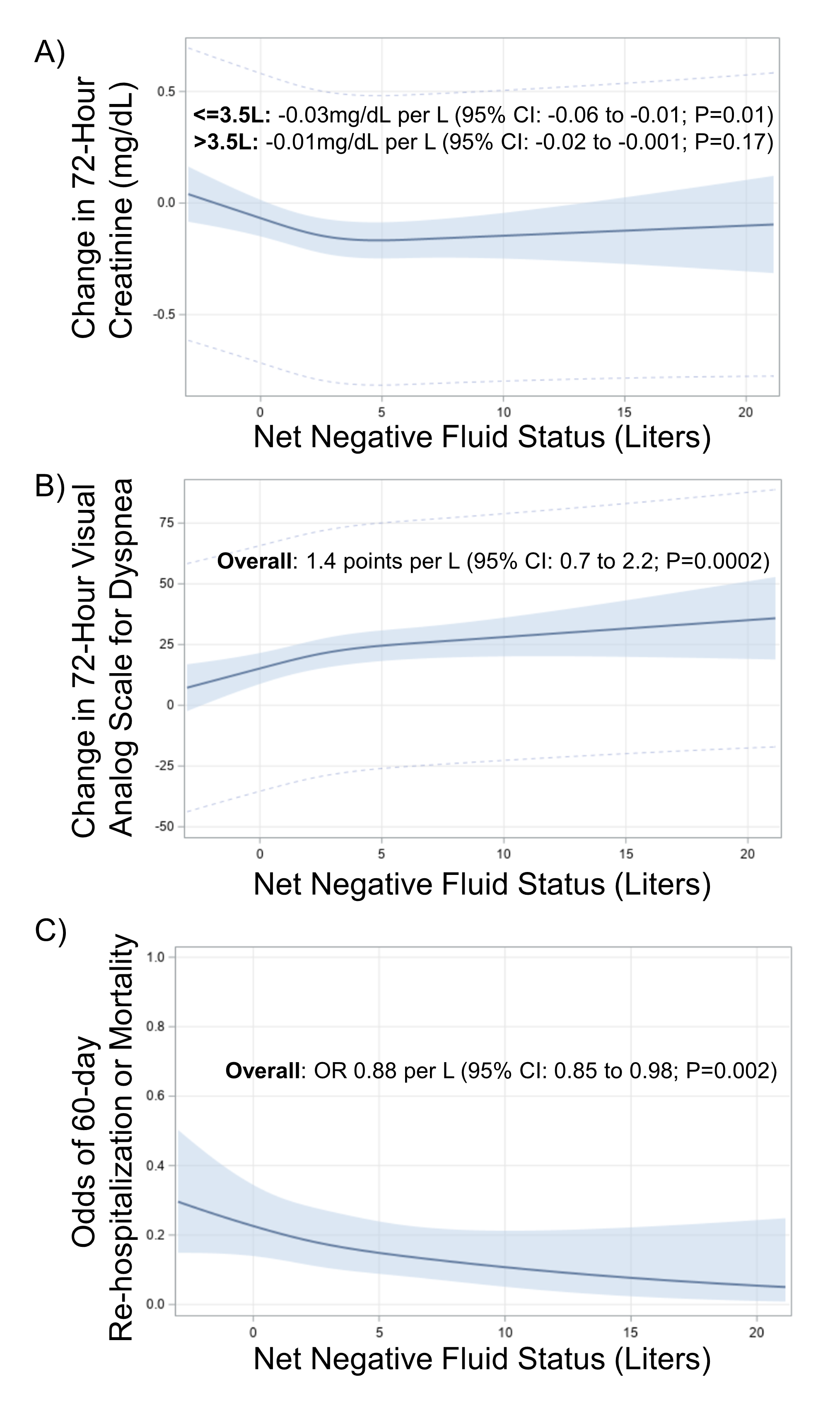
Methods: We conducted a pooled cohort study using data from three acute heart failure trials (DOSE, ROSE, and ATHENA-HF). All patients were initially eligible but were excluded if they had incomplete data for net fluid status, creatinine, or visual analog scale for dyspnea at baseline and 72 hours. From each cohort, we extracted patient demographics, comorbidities, vital signs, total furosemide dose, net fluid status, creatinine and dyspnea change, and mortality or re-hospitalization outcomes.The primary exposure was 48-hour net fluid status. The co-primary outcomes were 72-hour changes in creatinine and dyspnea. Net fluid status was divided into quartiles and multiple linear regression models were constructed to evaluate the association of net fluid status and each co-primary outcome, adjusting for relevant covariates. We explored the potential for a non-linear relationship between net fluid status and each co-primary outcome by performing a restricted cubic spline with knots at 10th, 50th, and 90th percentiles. We visually inspected the splines for inflection points to use as cut-off points. If a non-linear trend was observed, we modeled net fluid status as two piecewise segments above and below the inflection point with segmented linear regression. In a secondary analysis, a multiple logistic regression model was constructed to evaluate the association of net status and 60-day re-hospitalization or mortality. Non-linear relationships were also visualized using cubic splines.
Results: 807 patients were included (244 from DOSE, 316 from ROSE, 247 from ATHENA-HF). The mean age was 67 years and 27% were female. In the cohort, 52% had diabetes, 82% had hypertension, 24% had COPD, 51% had a prior pacemaker or defibrillator, and 61% had cardiac arrhythmias. The median ejection fraction was 30%. The mean 48-hour net status was -2.9L. In the fully adjusted linear regression, there was a statistically significant reduction in 72-hour creatinine in Q3 compared to Q1 (Table 1). The effect estimates for Q2 and Q4 were quantitatively similar as Q3 but did not meet statistical significance. A non-linear association was observed with net fluid status and creatinine change, such that creatinine improved with each liter net negative up to 3.5L (-0.03 mg/dL per liter negative, P=0.01) and remained stable beyond 3.5L (-0.01 mg/dL per liter negative, P=0.17) (Figure 1A). Net fluid loss quartile was associated with a monotonic improvement in dyspnea (Q2 vs Q1: 2.3; Q3 vs Q1: 6.2; Q4 vs Q1: 12.6). (Table 1). We visualized a linear trend in net fluid status and dyspnea improvement, such that each liter net negative was associated with an improvement in dyspnea score of 1.4 points (P=0.0002) (Figure 1B). In a secondary analysis, each liter net negative by 48 hours was also associated with 12% decreased odds of 60-day re-hospitalization or death (OR 0.88; 95% CI, 0.82-0.95; P=0.002) (Figure 1C).
Conclusions: In this pooled cohort of acute heart failure trials, we find that greater 48-hour net fluid loss was associated with improvements in 72-hour creatinine and dyspnea as well as reduced 60-day re-hospitalization and mortality risk. Future strategy trials should be conducted to evaluate the efficacy and safety of aggressive diuresis targets.