Background: Subspecialty consultation among hospitalists varies significantly across and within hospitals. While in many cases consultation is clinically necessary, in other cases it may represent overuse. Recent studies have explored predictors of consultation using observational administrative and EHR data. Qualitative methods may generate knowledge about additional factors and complex processes influencing consultation behavior not ascertainable from these sources. Our objective was to understand how pediatric hospitalists of different consultation intensities make decisions about subspecialty consultation.
Methods: This study took place at a large academic children’s hospital. We conducted semi-structured interviews, informed by the Social Ecological Model, with a purposive sample of high-consulting (top quartile) and low-consulting (bottom quartile) pediatric hospitalists previously identified through quantitative methods. Interviews were conducted virtually and audio recordings were transcribed. Two researchers coded transcripts using an integrated approach and established high interrater reliability (K > 0.75). Findings were organized by thematic categories derived from the Social Ecological Model.
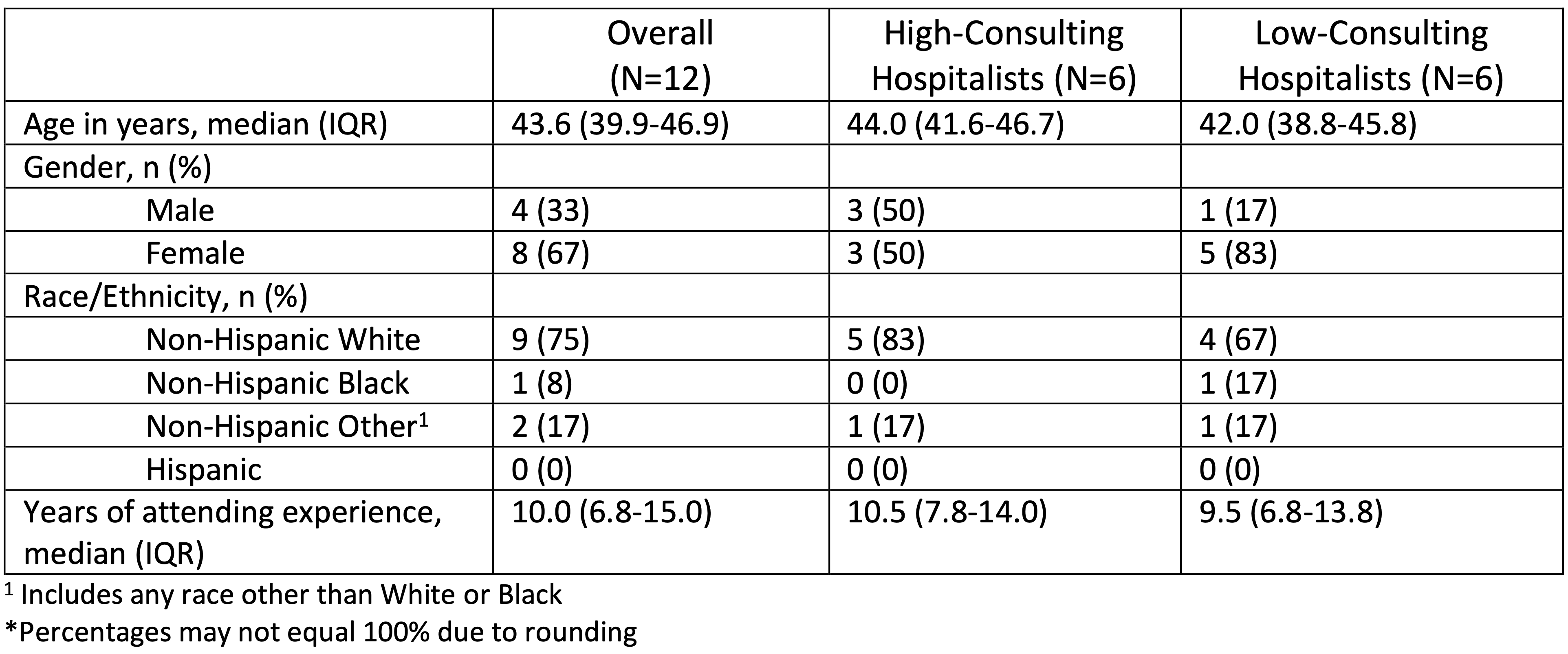
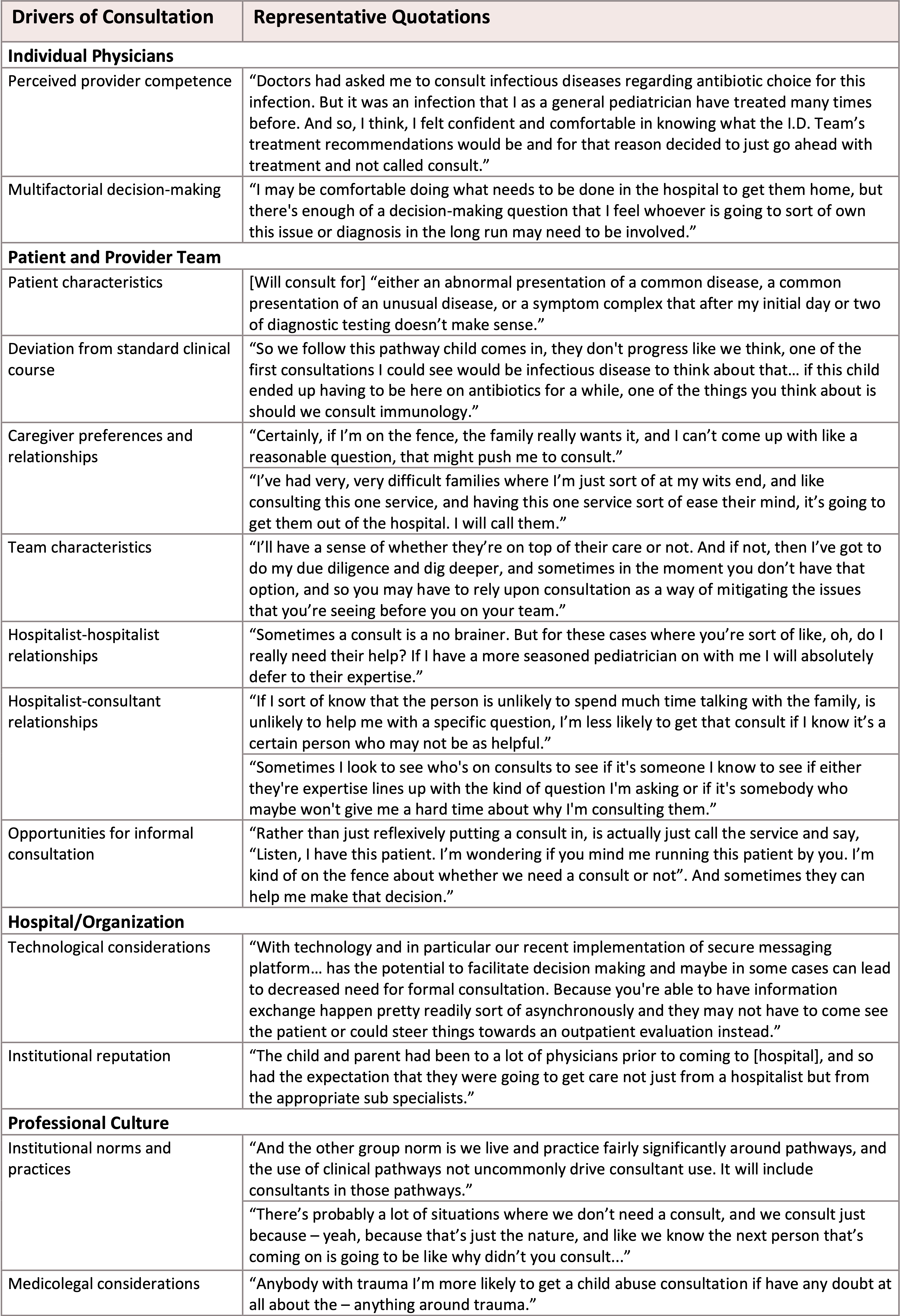
Results: Participants (n=12) included high- (n=6) and low- (n=6) consulting pediatric hospitalists. Characteristics of participating hospitalists are displayed in Table 1. In describing their decision to request consultation our respondents identified a number of considerations including patient characteristics such as medical complexity, previous patient relationships with subspecialists, and deviation from expected clinical course. Our respondents view their decisions to request consultation as being strongly influenced by a desire to maintain a relationship with the patient’s family, and family expectations. Specific to this context, the hospital’s elite reputation was believed to influence families to expect subspecialty consultations. Other considerations included medicolegal risk, confidence in their own competence and that of their colleagues on service, and helpfulness of consultants. Respondents suggested that aspects of the hospital’s information systems facilitate consultation by making the process easier, including secure text message communication and clinical pathway order sets. Specific factors that make hospitalists less likely to request consults include a proficient clinician team, easy access to experienced hospitalists, and “curbsiding” subspecialists to determine the necessity of a formal consult. High-consulting hospitalists were more likely to describe medicolegal concerns, institutional norms and caregiver preferences than low-consulting hospitalists. Exemplar quotations demonstrating each finding are provided in Table 2.
Conclusions: Decision-making around subspecialist consultation is multifactorial and influenced by factors not related to a patient’s clinical need. Our findings suggest that future efforts to reduce low-value consultation will need to take into consideration the social and organizational dynamics that promote consultation.