Background: Background: Ultrasound has diagnostic value at the point-of-care among hospitalized patients. In COVID-19 pneumonia, lung ultrasound has been used as a diagnostic and prognostic tool. For example, using the results of nasal PCR test as the reference standard, a modified lung ultrasound score (LUS) ≥ 8 is highly predictive of COVID-19. However, a focused evaluation of the heart and IVC may improve the diagnostic accuracy among patients presenting with undifferentiated respiratory failure.
Methods: This prospective cohort study involved patients admitted under investigation for COVID-19 between April 28th – August 2nd 2020. Our primary outcome measure was a positive nasal PCR test for COVID-19. To be included patients needed to have an initial nasal rt-PCR swab for SARS-CoV-2 obtained within 24 hours of study enrollment. Additional inclusion criteria required that patients have respiratory symptoms (cough or dyspnea), objective fever (temperature of at least 38°C), hypoxia (pulse oximetry less than 94%) or change in baseline oxygen requirements without a clear alternative diagnosis. Exclusion criteria included skin abnormalities or bandaging preventing ultrasound probe placement, severe agitation or imminent death. Patients underwent a 10-field lung ultrasound and a cardiac scan consisting of the four cardinal windows and an assessment of the IVC. Images were interpreted independently by two separate study personnel, one of whom was blinded to the PCR result
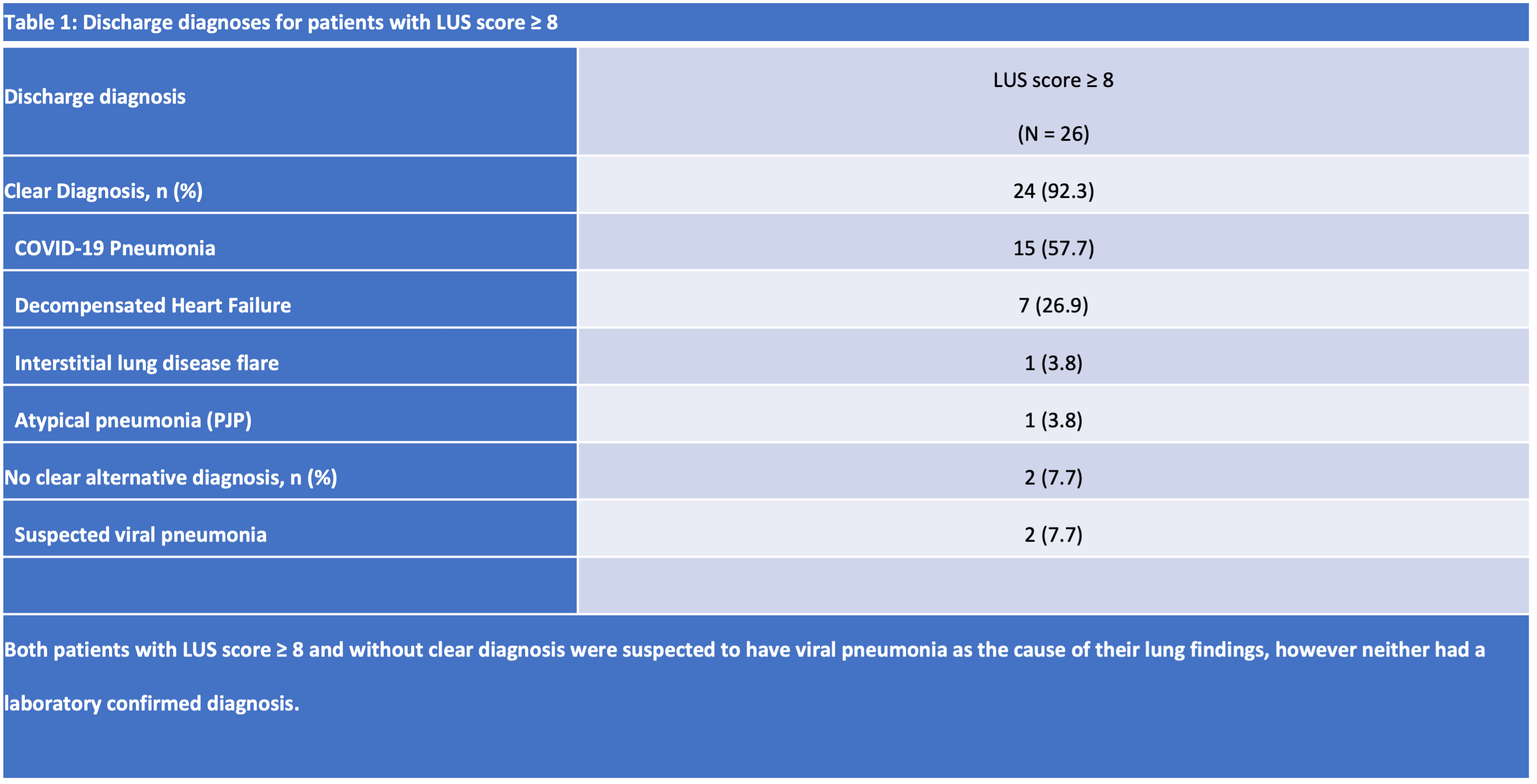
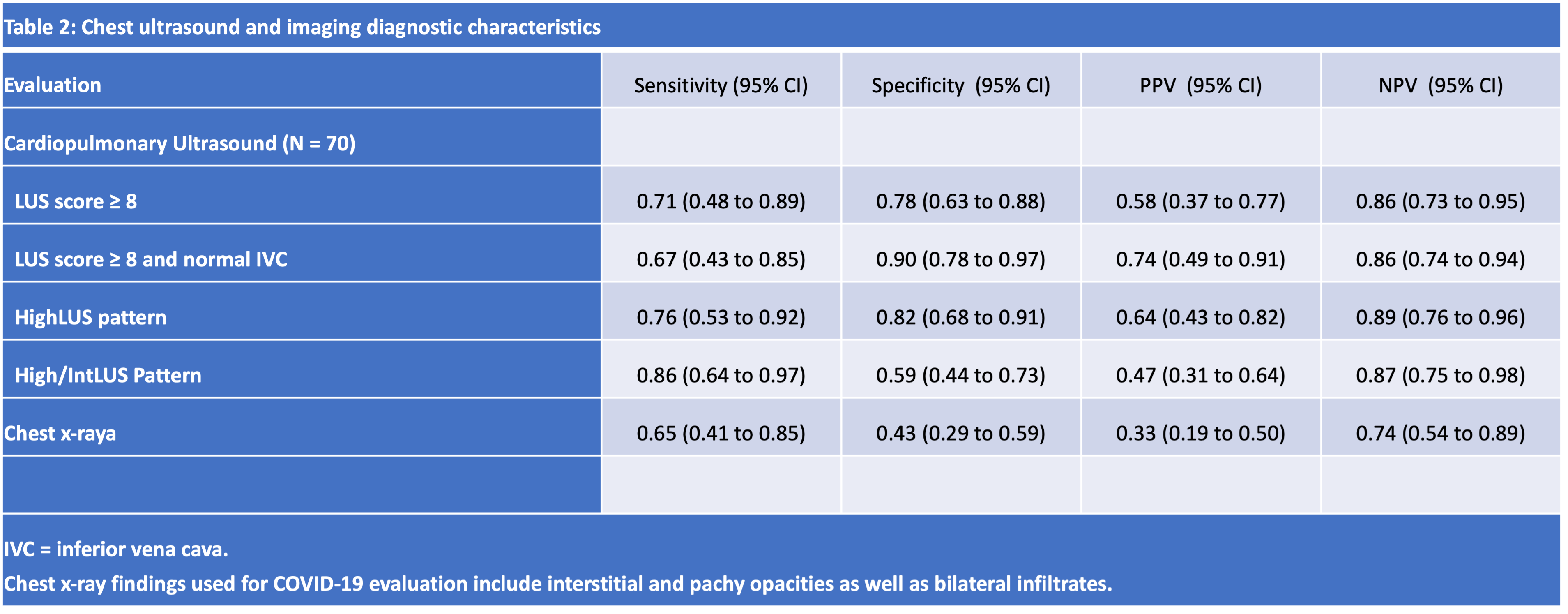
Results: Seventy participants were enrolled and completed the ultrasound protocol. Of these patients 21 (30%) tested positive for SARS-CoV-2 by PCR and 49 tested negative (70%). Of the 52 patients who initially tested negative 31 (60%) were retested after 48 hours and 3 (6%) tested positive. There were 26 of 70 patients with a modified LUS ≥ 8. Eighteen (69.2%) were found to have an “atypical” pneumonia (15 with COVID, 1 with PCP and 2 without a clear etiology), 7 (26.9%) were found to have decompensated heart failure and 1 (3.8%) was found to have an ILD flare. A modified LUS score of 8 or greater demonstrated a diagnostic AUC for COVID-19 of 0.73 (CI, 0.6 to 0.87). Inclusion of IVC assessment improved the diagnostic accuracy of a LUS score of 8 or greater from 0.73 (CI, 0.64 to 0.85) to 0.83 (CI, 0.72 to 0.91), primarily leading to improved specificity.
Conclusions: Numerous studies have confirmed the utility of lung ultrasound in the diagnostic evaluation of COVID-19 pneumonia. However, a smaller number have quantified the value added from a systematic evaluation of multiple bedside cardiac views. Our study demonstrates that among a sample of symptomatic patients under investigation for COVID-19 pneumonia, a well-executed lung ultrasound in conjunction with examination of the IVC can augment the diagnostic evaluation primarily through increasing specificity. While certain ultrasonographic findings have been strongly associated with COVID-19, these are not pathognomonic. Our study highlights a representative differential diagnosis for the lung artifacts observed and further supports the importance of using bedside ultrasound in conjunction with clinical impression in the work-up of hospitalized adults with respiratory failure.