Background: Asymptomatic bacteriuria (ASB), the presence of bacteria in urine without signs or symptoms of a urinary tract infection, is a common finding. The current recommendation by the Infectious Diseases Society of America is against screening for and treating ASB in patients undergoing non-urologic surgeries, due to the lack of demonstrable benefit in reducing the risk of surgical site or prosthetic joint infection. Despite this, the existing practice at UC San Diego (UCSD) has been to recommend a preoperative urinalysis (UA) on every patient undergoing an orthopedic surgical intervention. The goal of this project is to quantify the rate of this low-value practice and identify opportunities for antibiotic stewardship.
Methods: A retrospective chart review was conducted of patients admitted to UCSD to undergo surgical repair of hip or femoral fractures from January to December of 2020. Data elements abstracted included a documented recommendation for a screening UA, rates of positive UA and/or urine culture, and whether antibiotics were administered. Baseline rates of screening UAs ordered were calculated, as well as rates of positive urine cultures and antibiotic administration to those with ASB. Charts were also reviewed to identify any immediate complications resulting from antibiotic administration (e.g. C. diff infections, adverse drug reactions) as well as complications from withholding antibiotics for ASB (e.g. prosthetic joint infections, wound infections).
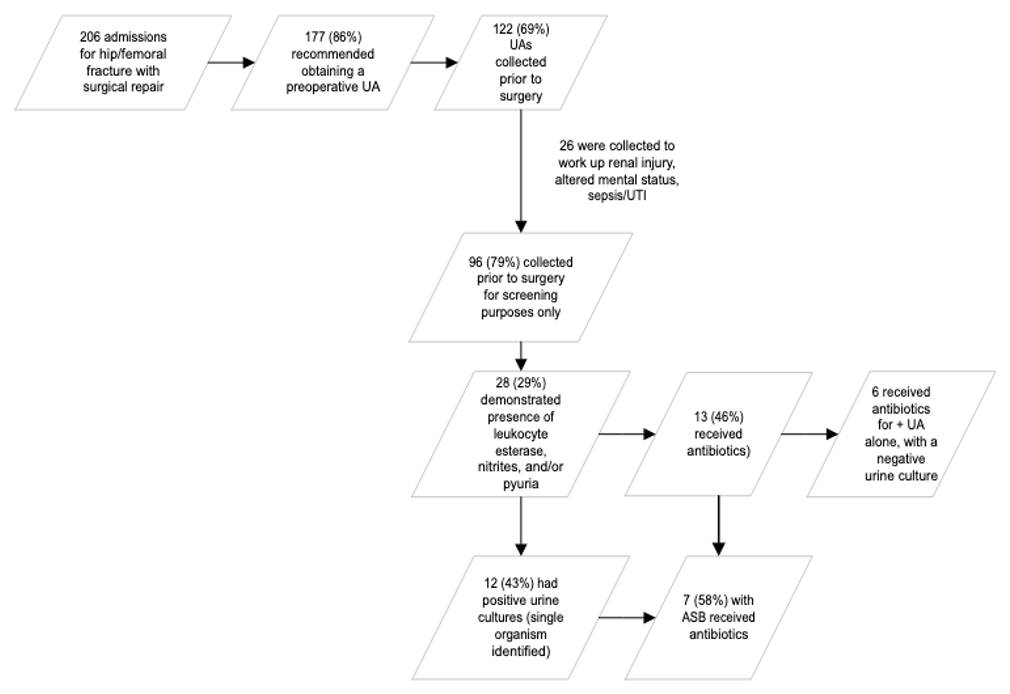
Results: Of 206 cases admitted for surgical intervention of a hip/femoral fracture, 177 (86%) recommended obtaining a preoperative UA. 122 (69%) had a UA collected prior to surgery. Excluding those collected to work up altered mental status, renal injury, or clinical suspicion of infection, 96 (79%) cases were identified in which a UA was collected for screening. 28 (29%) UAs were “positive,” defined as presence of leukocyte esterase, nitrites, or pyuria. 12 resulted in a positive urine culture, 7 of which received antibiotics to treat the bacteriuria. Additionally, 6 patients received antibiotics for a positive UA despite having a negative urine culture. There were no identified complications within 30 days of receiving antibiotics, nor any from untreated ASB.
Conclusions: This study confirmed a high rate of screening UA recommendations prior to orthopedic surgeries despite the lack of evidence to support this practice. While only 12 cases of ASB were identified, 7 received antibiotics perioperatively to treat the bacteriuria, a treatment rate of over 50%. Furthermore, half of those who received antibiotics were being treated based on UA results alone despite a negative urine culture. Four of those who received treatment for ASB received a single dose of antibiotics preoperatively, despite the lack of evidence to support the use of single-dose antibiotic prophylaxis prior to non-urologic procedures. This study is limited by a small sample size and reliance on accurate documentation within a single electronic medical record within a limited time frame. Despite these limitations, it reveals multiple areas for improvement in education, resource utilization, and antibiotic stewardship.