Background: The CDC recognizes antimicrobial resistance as an urgent global public health threat and supports antibiotic stewardship initiatives to combat antibiotic resistance. Pneumonia is a frequent condition treated by both hospitalists and emergency room physicians and the most common reason for inpatient antibiotic use and over prescribing. Recent IDSA guidelines for the treatment of community acquired pneumonia support a 5 day course of antibiotics for patients with uncomplicated pneumonia, joining the growing evidence supporting a “shorter is better” mentality for many infectious conditions. However, up to two thirds of patients admitted with community acquired pneumonia receive excess antibiotic therapy, resulting in increased risk for antibiotic associated adverse events.
Purpose: At our institution, a multi-hospital system composed of tertiary care centers, community and critical access hospitals, we found that adults with community acquired pneumonia discharged home from the emergency department or admitted to the inpatient hospitalist services primarily received unnecessarily prolonged courses of antibiotics. The aim of this initiative was to increase the percentage of patients with community acquired pneumonia who received 5 total days of antibiotics from less than 50% to 75% or greater following our intervention periods (Oct-Dec 2020 and Dec 2021-Jan 2022 ) and sustain our improvements for at least 6 months.
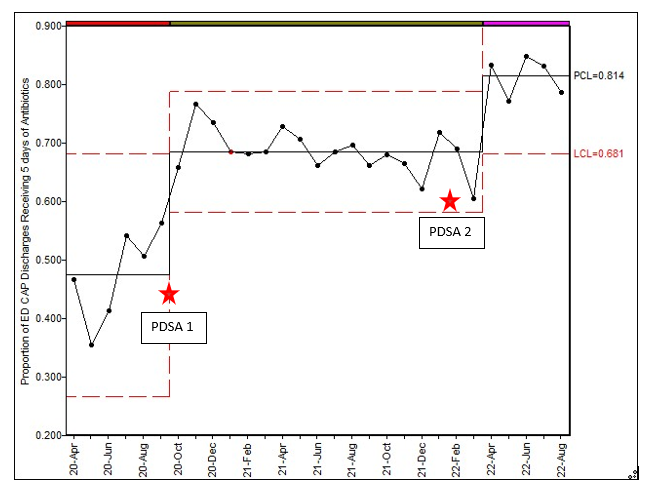
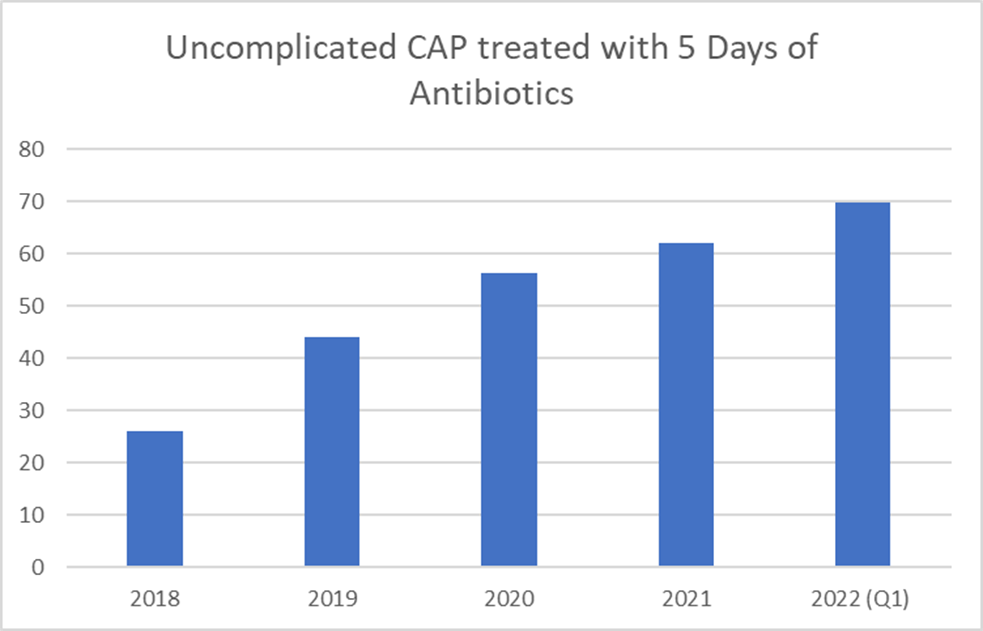
Description: In collaboration with emergency department leadership, hospitalists teams, and the antibiotic stewardship program, we designed and implemented a community acquired pneumonia stewardship initiative. Education was provided to Emergency Department and Hospitalist teams including attendings, resident physicians, and APPs. Additional electronic medical record tools were implemented to optimize viewing of antibiotic durations at the time of discharge, and ordersets with clinical decision support were created to encourage 5 day antibiotic durations and appropriate antibiotic selection including for those patients with listed penicillin allergies. Baseline performance data was shared with both teams. (PDSA 1). We subsequently designed a clinical practice guideline focusing on antibiotic prescribing recommendations for pneumonia including selection and duration of antibiotic therapy, provided additional provider education, and supplied feedback to underperforming areas. (PDSA 2). Following implementation, the percentage of adult patients with pneumonia discharged from the emergency department receiving a 5 day course of antibiotics increased from approximately 47% to 68%, and sustained improvement for greater than 12 months (Figure 1), followed by additional improvements after PDSA cycle 2. We also observed an improvement in the percentage of eligible inpatients on the hospitalist service receiving 5 days of antibiotics from approximately 45% to 70% (Figure 2).
Conclusions: Applying our antibiotic stewardship intervention to the problem of unnecessary antibiotic durations in community acquired pneumonia resulted in significant improvements in the percentage of adult patients discharged from the emergency department receiving a 5 day course of antibiotics. We also found an increase in the percentage of eligible adult inpatients on the hospitalist service receiving 5 total days of antibiotic therapy. This project represents a unique implementation of a successful joint hospitalist and emergency department quality improvement initiative.