Background: Hospitalist-run Medical Procedure Services (MPS) have been shown to decrease time-to-procedure, overall length of stay, and interventional subspecialty consults for bedside procedures while increasing revenue for hospitalist groups [1,2,3,4]. However, significant challenges remain in the deployment of a financially sustainable MPS, and there is interest in identifying and deploying strategies to improve sustainability. Two such strategies, including appropriate utilization of point-of-care ultrasound (POCUS) for both procedure guidance and bedside diagnosis and leveraging the MPS’s availability for challenging-to-coordinate procedures such as tPA/Dornase treatments for empyema, offer opportunities to increase MPS revenue while improving patient care.
Purpose: To describe the impact of implementation of a series of interventions on procedure volumes and charges billed by an MPS at a tertiary care academic medical center. The interventions included increasing utilization and proper documentation of ultrasound guidance for procedures, billing for diagnostic POCUS exams performed when no procedure is indicated (i.e. “no fluid” exams), and introducing new procedures such as tPA/Dornase administration to pleural drains.
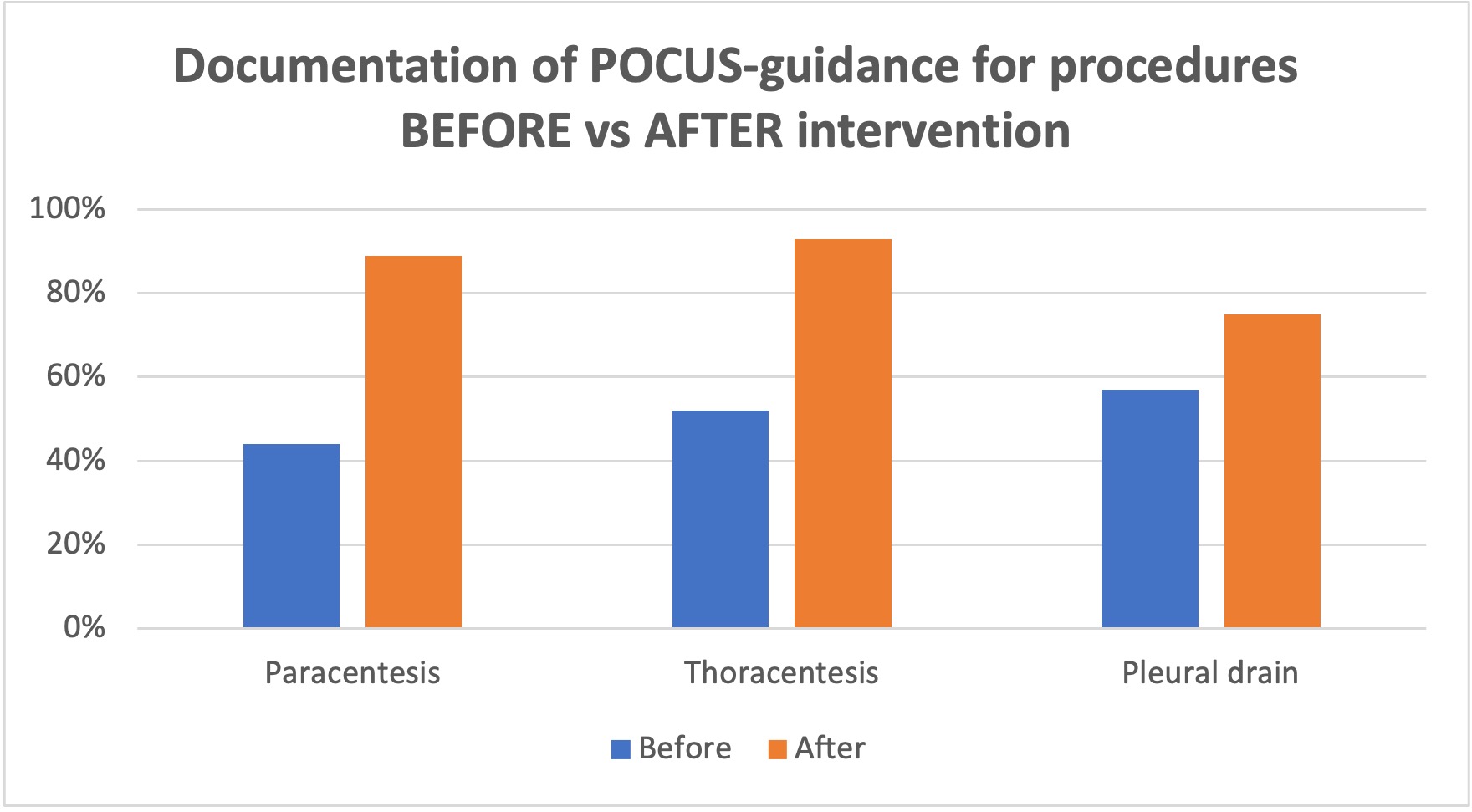
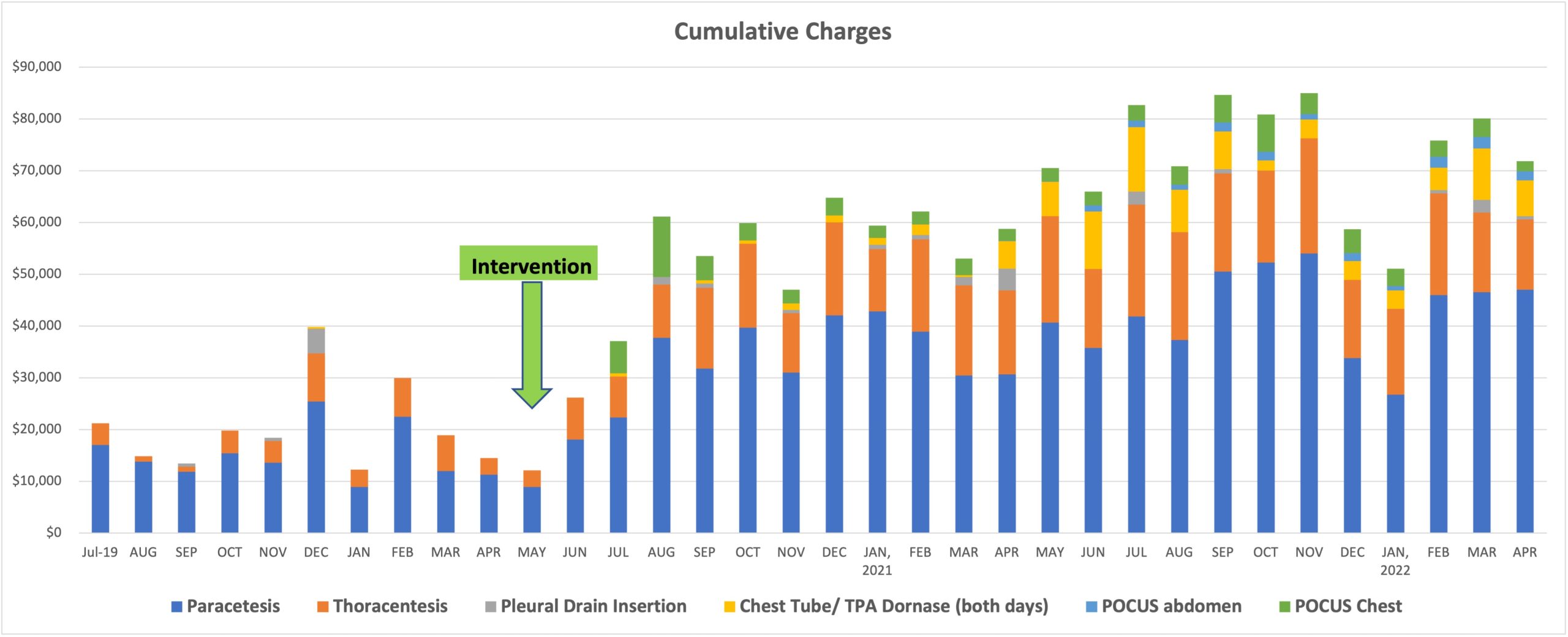
Description: A retrospective analysis was conducted by compiling de-identified billing data from the MPS on procedure volumes and charges billed between July 2019 and April 2022. Data from 2,228 procedures and 940 diagnostic POCUS studies were analyzed to evaluate billing and collections before and after each intervention. There was a significant increase in documentation of ultrasound guidance for paracentesis (45%), thoracentesis (41%), and pleural drain insertion (18%). Total volume of procedures also increased during this time, with the average number of paracentesis performed per month increasing from 24 to 45 and thoracentesis increasing from 9 to 24 (Figure 1). The combination of increased volume and improved documentation of POCUS-guidance resulted in a greater-than two-fold increase in annual charges for paracentesis ($178,881 to $430,092) and thoracentesis ($48,290 to $185,174). The addition of diagnostic POCUS exams and administration of tPA/Dornase to pleural drains also provided substantial increases in revenue streams for the MPS, with diagnostic chest and abdominal POCUS exams generating $87,413 and $16,638 respectively (a combined $104,051), and $93,274 for tPA/Dornase administration to pleural drains (Figure 2).
Conclusions: An iterative series of interventions increased the financial profitability and sustainability of the Hospitalist MPS. This was accomplished by emphasizing the importance of proper documentation of POCUS guidance for procedures, increasing the availability of POCUS devices, and most importantly, optimizing the electronic medical record system to provide physicians a more efficient process for recording and uploading POCUS images. These interventions were common sense, good for patient care, and have a low barrier to adoption.