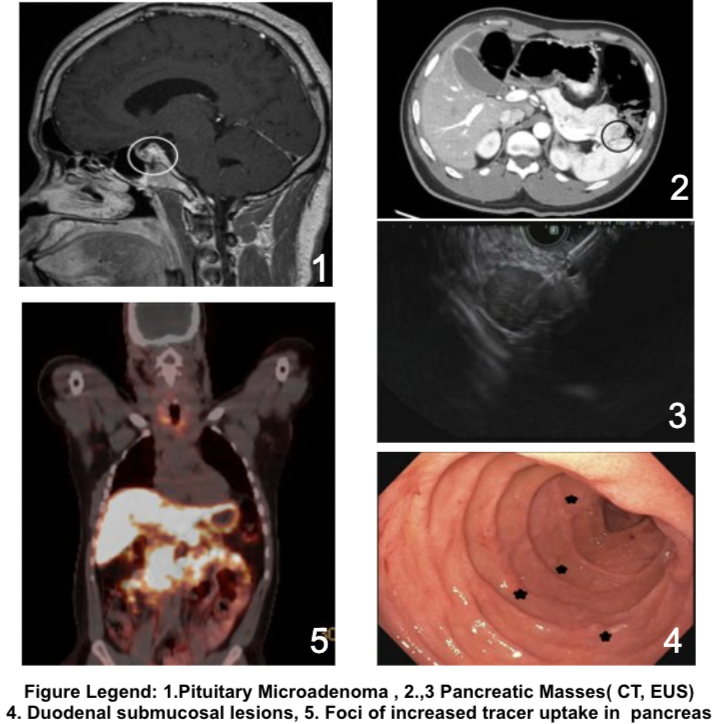
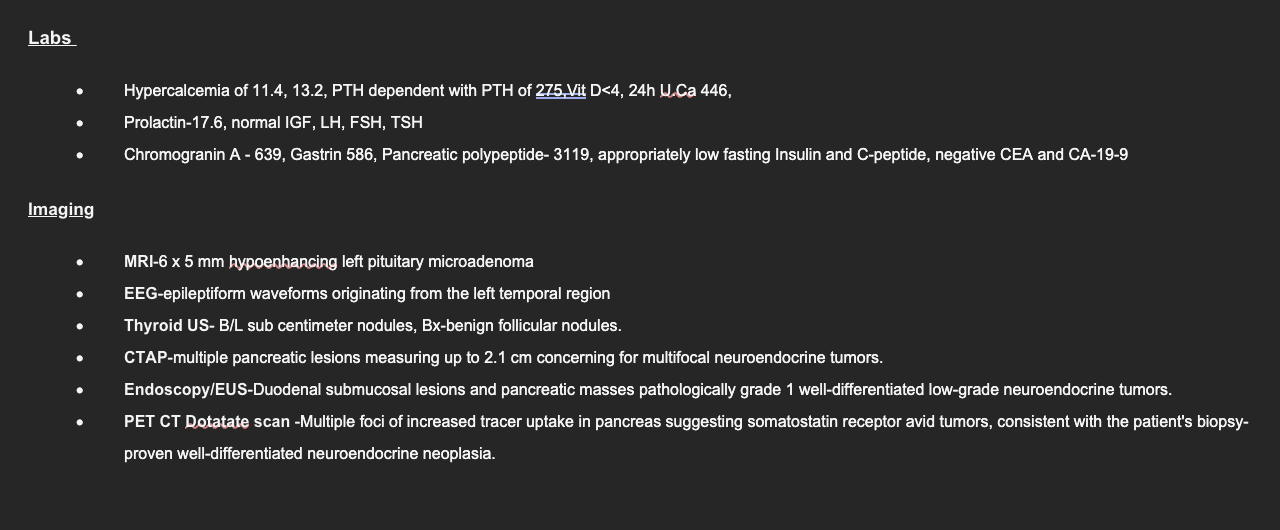
Case Presentation: A 29-year-old man was brought to our emergency department with a new-onset witnessed seizure. He was recently prescribed oral omeprazole for heartburn. He had no known medical conditions but had a family history of MEN1 in his father and paternal uncle. Initial labs showed hypercalcemia, with elevated PTH. MRI brain showed a sub-centimeter pituitary microadenoma with no acute intracranial abnormality. Video EEG showed a focal epileptogenic zone in the left temporal and central regions. Seizures were controlled with levetiracetam and lacosamide. Given his family history, these findings were consistent with familial MEN1. His epilepsy was deemed to be unrelated to his MEN1 due to lack of coexisting hypoglycemia with seizures.He was discharged but soon readmitted for heartburn, nausea, and vomiting. In the setting of presumed MEN1, further workup showed elevated gastrin and chromogranin levels. CT scan of the abdomen was obtained for concern for neuroendocrine tumors (NETs), which showed multiple duodenal and pancreatic lesions. Upper GI endoscopy with endoscopic ultrasound showed multiple duodenal lesions and pancreatic masses, which were confirmed to be well-differentiated NETs on biopsy.For his symptomatic hypercalcemia, he underwent outpatient subtotal parathyroidectomy. He was recommended annual follow-up with brain MRI. He was also started on lanreotide, a somatostatin analogue to arrest further growth of tumor lesions. Consideration for surgical enucleation of duodenal lesions with partial pancreatectomy is currently underway.
Discussion: We present a classic case of MEN 1 in a patient with significant family history with the presence of primary hyperparathyroidism, pituitary microadenoma, and duodeno-pancreatic NETs. Interestingly, rare presentations of MEN1 as refractory seizures have been reported secondary to hyperinsulinemic hypoglycemia, but our patient was euglycemic with appropriate levels of insulin and C-peptide. This suggests an alternative etiology that is not well documented in the available literature . Given the complex and highly specialized skills needed to diagnose and treat MEN1, the involvement of a multidisciplinary team is vital.
Conclusions: When the clinical suspicion for MEN1 is high, endocrinology evaluation with appropriate laboratory workup and targeted imaging of the typical endocrine organs as described for this patient are advised with careful multidisciplinary management and follow-up.