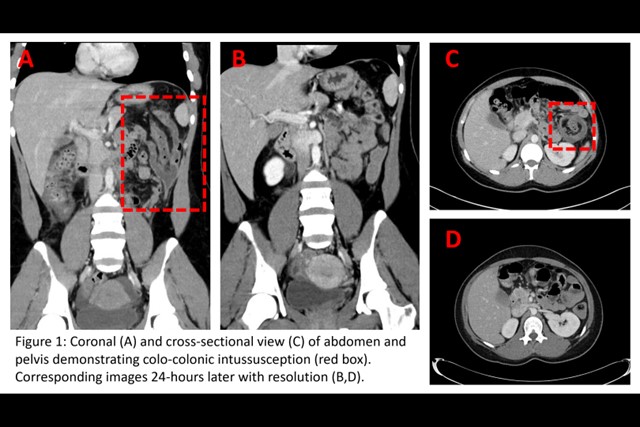
Case Presentation: Hereditary angioedema (HAE) is an uncommon diagnosis, but one with which providers should be familiar. While most frequently associated with localized edema of extremities and face, it may also present with gastrointestinal manifestations. Viral infection, including SARS-CoV-2 infection, can be one of many triggers for angioedema exacerbation. Here we present the clinical vignette of a 26-year-old patient hospitalized for intussusception secondary to colonic angioedema in the setting of a SARS-CoV-2 infection. Patient presented to ED with abdominal pain, nausea, vomiting. CT imaging revealed colo-colonic intussusception involving transverse and descending colon without obvious lead point or mass (Figure 1 a,c). Labs revealed a positive SARS-CoV-2 PCR. She was treated with supportive care with resolution of intussusception and improvement of symptoms (Figure 1 b,d). 48-hours later, she re-presented to care with rapid onset generalized swelling of hands (Figure 2). Further work-up revealed low C4 complement levels, and low levels of function and protein of C1 inhibitor, consistent with a diagnosis of hereditary angioedema (HAE). She underwent a colonoscopy finding no evidence of colitis, mass, or other explanation for intussusception. On follow up, she continued to have intermittent episodes of abdominal pain and vomiting but has had symptomatic improvement with treatment with subcutaneous C1 inhibitor for prophylaxis and anti-bradykinin antibody for breakthrough symptoms.
Discussion: Here we review the case of a young and otherwise healthy patient who presented to care with intussusception and upper extremity swelling secondary to HAE in the setting of an asymptomatic SARS-CoV-2 infection. HAE is a rare autosomal dominant disorder characterized by decreased C1 inhibitor activity. In the setting of a physiologic stress activating the complement cascade, failure to adequately inhibit the protease kallikrein by C1 inhibitor leads to excess conversion of high molecular weight kininogen into bradykinin, triggering vasodilation and tissue edema(1). Patients with HAE most commonly present with recurrent episodes of self-resolving cutaneous angioedema, characterized by non-pitting, non-pruritic swelling of skin or mucous membranes, and less commonly with laryngeal edema. HAE may also present with gastrointestinal manifestations, most commonly intermittent abdominal pain, caused by intestinal edema(2-6). Intussusception secondary to gut wall edema has been reported in HAE(7-9), and usually resolves with non-surgical management and HAE-directed therapies. SARS-CoV-2 virus infection is known to trigger an immune response via the complement cascade10 and has been reported to trigger a flare of symptoms in patients with HAE(11-13). Belbézier, et al report 31% of their HAE patient cohort experienced an angioedema attack with concurrent COVID-19 infection. Thus, suspicion for HAE must be particularly high during the COVID-19 pandemic.
Conclusions: Recurrent abdominal pain is a common reason for admission to a hospitalist service. HAE is a rare diagnosis, but one that should be considered in a patient with recurrent, unexplained swelling or gut edema. It can be readily diagnosed using complement levels and C1 inhibitor protein and function assays. In patients presenting with intussusception, symptoms can often resolve with non-surgical management. COVID-19 infection can trigger angioedema attacks in patients with HAE.