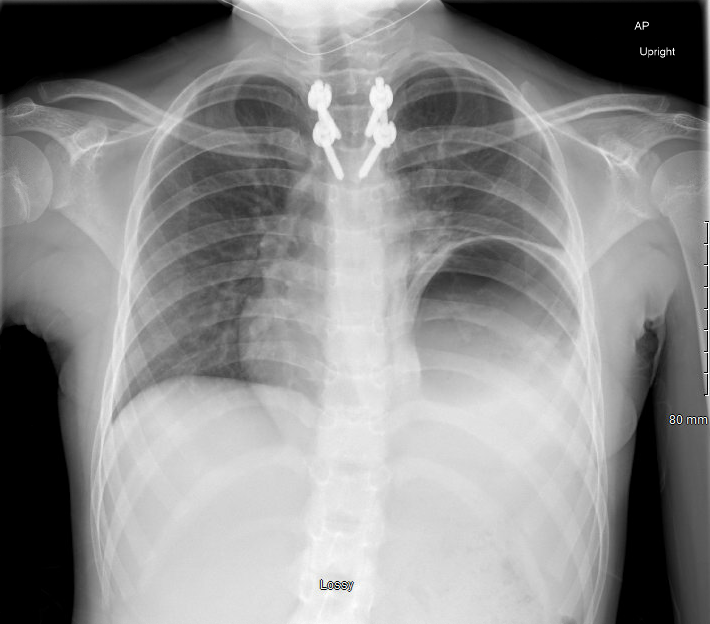
Case Presentation: An 11-year-old female with history of T4 paraplegia after an MVC requiring extensive intrabdominal surgical intervention, neurogenic bowel and bladder and malnutrition presented to the ED with intractable vomiting and left shoulder pain. Acute vomiting started earlier in the day while she was being straight catheterized as per routine and continued throughout the day until she was unable to tolerate food or liquids. Left shoulder pain started the day prior and worsened when lying flat. On physical exam, she was hypertensive and tachycardic, but otherwise hemodynamically stable and in no acute distress. Cardiovascular exam revealed regular rate and rhythm with 2+ peripheral pulse and cap refill < 2 seconds. She had some shortness of breath but was not in respiratory distress and clear to auscultation bilaterally. On exam, her abdomen was soft, non-tender and nondistended. Multiple well healed scars could be appreciated from her past abdominal surgeries. Hyperactive bowel sounds were noted. Neurological exam was notable for baseline paraplegia and absent sensation of lower extremities. Abdominal X-ray showed severe constipation with large amount of stool over the entire colon. Chest x-ray showed stomach bubble elevated into the left chest, suggesting elevation of the left hemidiaphragm but otherwise, no other acute lung findings. Right upper quadrant ultrasound was within normal limits. Once admitted, she was started on a bowel cleanout. Oral cleanout was attempted at first, but she did not tolerate it and was switched to an NG cleanout. By day 3 of admission, she completed her clean out and was restarted on a regular diet with initial resolution of symptoms. However, as time continued, she resumed having emesis and inability to tolerate PO attempts despite repeat abdominal x-ray showing no signs of remaining constipation. Upper GI with small-bowel follow through was obtained and it showed organo-axial gastric volvulus as the cause of her intractable vomiting.
Discussion: Organo-axial gastric volvulus means the stomach is twisting along its long axis. It is rare and it can lead to gastric outlet obstruction. Gastric volvulus is more commonly seen in adults and is usually associated with diaphragmatic abnormalities. In pediatrics, it is more commonly seen in infants born with congenital diaphragmatic hernia. The patient and her parents revealed that she had been having nausea and decreased appetite for the past few months which would improve with Zofran and Cyproheptadine. It is presumed that this volvulus may have started to develop at that time which resulted in vague and non-specific symptoms. She was able to tolerate NG bowel cleanout most likely due to the force of the GoLytely opening the angle and allowing the fluid to pass through the stomach. However, once the cleanout was done, she again developed food and fluid intolerance. She was taken to the operating room where a small diaphragmatic hernia was discovered. She underwent reduction and detorsion of gastric volvulus, hernia was repaired, and a G-tube was placed to help anchor the stomach in addition to aid in her nutrition. Since the repair, the patient has been gaining weight appropriately and not complaining of any of her admitting symptoms.
Conclusions: In patients with history of multiple intrabdominal surgical interventions, it would be wise to consider organo-axial gastric volvulus in the setting of chronic constipation and left shoulder pain. An elevated hemidiaphragm on x-ray should also raise suspicion for diaphragmatic abnormalities.