Background: Coaching and mentorship programs for new hospitalists can help support early career development. However, new faculty may need additional real-time support as they attend on service for the first time. This may be particularly useful on the teaching service given the unique challenges new faculty may face, such as developing teaching points, providing feedback to learners, managing complex clinical scenarios, and navigating workflows at a new institution . In our large hospital medicine division of over 150 faculty providing care at four geographically distinct hospitals, it can be challenging for new faculty to identify support.
Purpose: To develop a peer mentorship structure to provide real-time support new hospitalists attending on the teaching service.
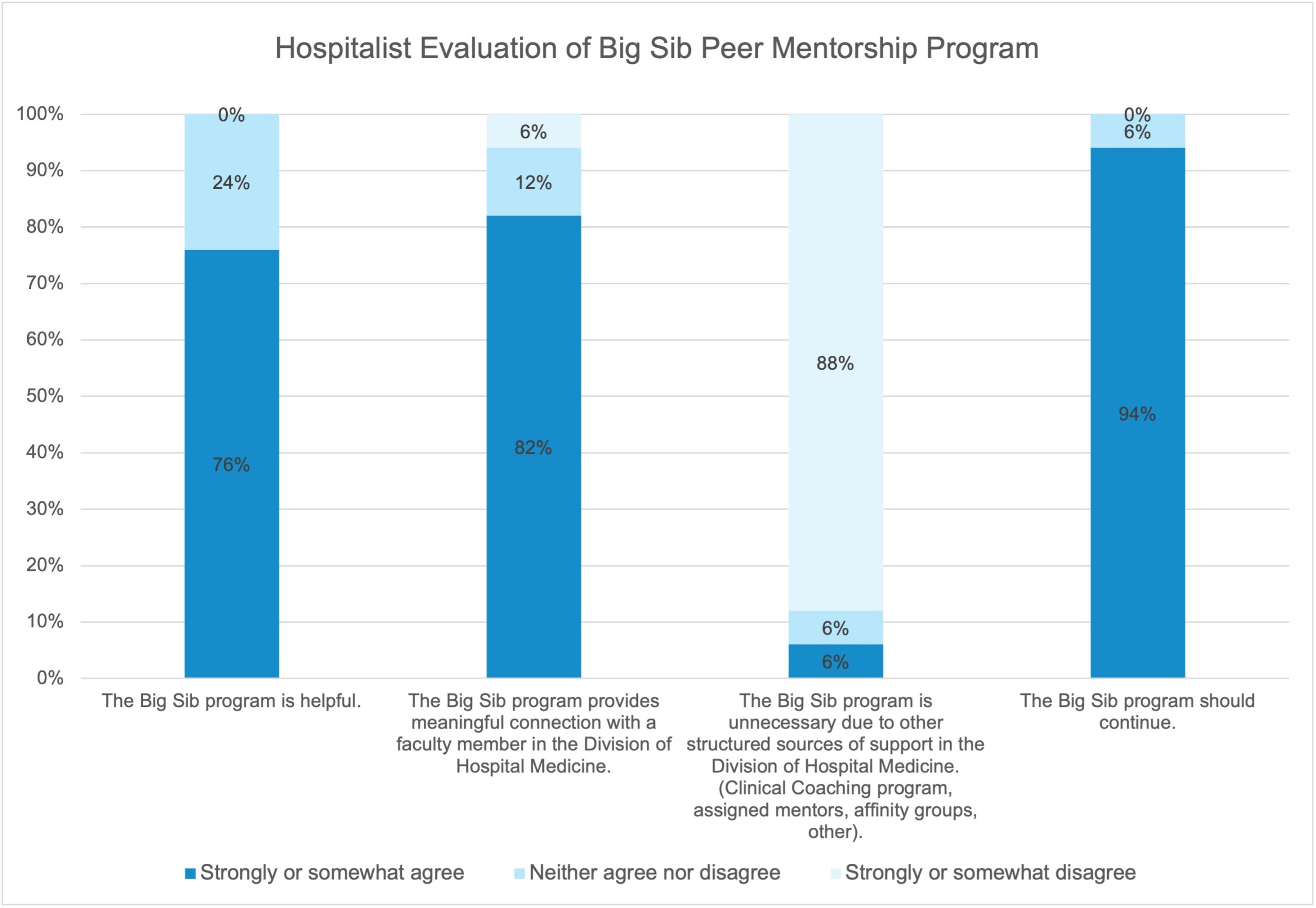
Description: We developed a peer mentorship program called the “Big Sib program” to support new hospitalist faculty and fellows during their first time attending on the hospital medicine teaching service. Approximately one week prior to the new faculty rotating onto service, service leaders identified other faculty who were scheduled to be attending on the teaching service during the same dates and invited a faculty member to serve as a peer mentor (“Big Sib”) via a personalized email. All invited faculty agreed to serve as Big Sibs (100% agreement rate). Big Sibs were provided with general guidance to assist new faculty with clinical, systems-related, or other questions. After Big Sibs were identified, service leaders introduced the new hospitalist to the Big Sib via a standardized email and briefly described the Big Sib program and expectations. Most Big Sibs exchanged contact information with new faculty. A few Big Sibs developed more formal mentorship structures and most provided ad hoc support. We surveyed first-year academic faculty and hospital medicine fellows regarding their experiences with the Big Sib program within 1 year of their start date. Our response rate was 55% (21/38); of respondents, 81% (17/21) reported being paired with a Big Sib during their first teaching block. Most (71%) new faculty reported meeting with their Big Sib 1-2 times during their time on service, with 18% meeting more than 2 times and 12% never meeting with their Big Sib. 82% of new faculty strongly or somewhat agreed that the Big Sib program provided a meaningful connection with a faculty member in the division of hospital medicine. Despite the availability of additional sources of structured support such as a clinical coaching program and assigned mentors, 76% of new faculty felt that the Big Sib program was helpful in addition to these programs and 94% agreed that the program should continue. Big Sibs provided general qualitative feedback that the time commitment to serve as a Big Sib was minimal and that they enjoyed the opportunity to meet and guide new faculty.
Conclusions: A “Big Sib” program successfully provided peer mentorship for new faculty and fellows on a hospital medicine teaching service. Peer mentors (“Big Sibs”) were eager to provide support to new faculty. The most challenging aspect of program implementation for our large hospital medicine group was keeping track of when new faculty were beginning their first rotation on the teaching service to proactively assign a Big Sib, particularly if faculty switched shifts after the start of the academic year or were jeopardized to the teaching service for their first blocks. This relatively simple, no-cost intervention could be easily implemented at other institutions to support new hospitalists.