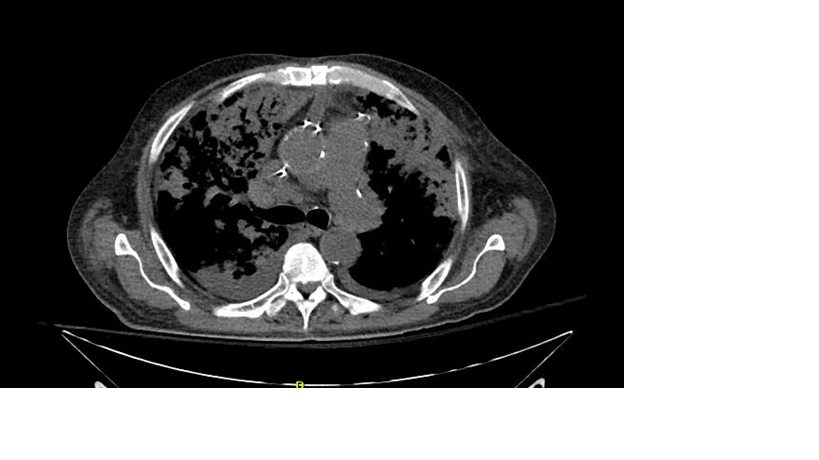
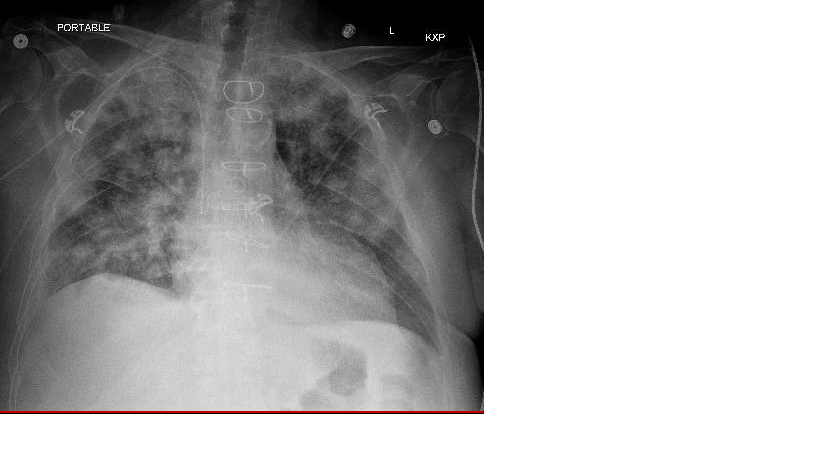
Case Presentation: A 67-year-old male with a past medical history of peripheral arterial disease, a chronic left lower extremity wound, and type 2 diabetes mellitus was admitted from vascular surgery clinic for osteomyelitis of the left lower extremity. He underwent multiple procedures by the podiatry service including a trans-metatarsal amputation. Intraoperative bone cultures returned positive for Enterococcus faecium and Candida albicans. The initial broad-spectrum antibiotics were switched to Daptomycin, Augmentin, and Fluconazole for a total of six weeks. Eight days after starting this regimen, the patient was noted to have dyspnea and hypoxemia requiring supplemental oxygen at 2L /hour via nasal cannula at rest. Lung exam revealed bilateral crackles. A complete blood count was notable for increasing leukocytosis 10.4 K/mcL (3.4-10.4 K/mcL). A chest radiograph demonstrated bilateral pulmonary opacities. Over the following three days the patient developed worsening hypoxemia requiring 15L/hour of supplemental oxygen by nonrebreather mask. Leukocytosis had increased to 14.6 K/mcL (3.4-10.4 K/mcL) with a differential notable for an eosinophil count of 0.55 K/mcL (ref 0.0-0.4 K/mcL). Computed tomography of the chest demonstrated bilateral upper lobe predominant extensive confluent consolidations and ground glass opacities consistent with advanced multifocal pneumonia. An extensive workup for infections was unrevealing and Daptomycin induced eosinophilic pneumonia was strongly suspected. Daptomycin was discontinued and the patient’s antibiotic regimen was changed. A course of glucocorticoids was initiated and the patient’s symptoms improved markedly, being able to wean off supplemental oxygen over two weeks.
Discussion: Daptomycin, a cyclic Linopeptide antibiotic, is utilized for targeted treatment for gram positive infections, including methicillin resistant staphylococcus aureus (MRSA) and vancomycin resistant enterococci (VRE). It is one of the most common drugs implicated in antibiotic associated eosinophilic pneumonia with an incidence between 1.7-4.8% [1-3]. The pathophysiology of daptomycin induced eosinophilic pneumonia is not well understood. Proposed mechanisms have included 1) an allergic reaction resulting in the release of inflammatory cells 2) epithelial injury from drug accumulation near the epithelial alveolar surface and 3) an inflammatory response triggered by altered lipid integrity as a result of the daptomycin-surfactant interaction [4, 5]. Symptoms typically arise 2-4 weeks after the initiation of daptomycin and include fever, hypoxia, and dyspnea. Imaging findings are notable for pulmonary infiltrates and/or ground glass opacities on chest radiograph or computed tomography. Diagnosis involves bronchoalveolar lavage to evaluate for eosinophils although peripheral eosinophilia has been proposed as a diagnostic criterion as well [4]. Treatment involves discontinuing the daptomycin as well as supportive care. The condition caries a favorable prognosis with early identification and drug discontinuation. Systemic therapy with glucocorticoids can also be helpful [2, 4, 6].
Conclusions: Daptomycin induced eosinophilic pneumonia is a rare condition characterized by hypoxia, dyspnea, and fever along with bilateral GGOs/lung opacities. Drug discontinuation, supportive care, and glucocorticoids are the mainstays of therapy. The condition carries generally good prognosis.