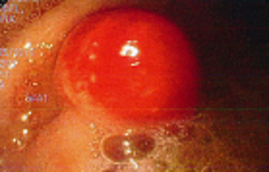
Case Presentation: A 43-year-old woman with controlled hypothyroidism presented to her primary care physician for evaluation of one-month of progressive fatigue, dizziness, and “disconnected” feeling. She noted decreased appetite leading to a twenty-pound weight loss. Following a benign physical examination, lab work demonstrated a striking macrocytic anemia with hemoglobin at 5.7 g/dL and mean corpuscular volume of 131 fL. Routine lab work two years prior was within normal limits. She was directed to our hospital for admission and evaluation. She did not regularly drink alcohol and noted no abnormal bruising or bloody stool. Manual differential demonstrated megaloblasts, anisopoikilocytosis, and macroovalocytes. She was found with a mildly decreased vitamin B12 of 127 pg/mL, folate of 18.31 ng/mL, and relatively benign iron studies. An elevated lactate dehydrogenase to 6158 U/L, low haptoglobin (unmeasurable), and total bilirubin of 1.7 mg/dL with normal direct, were highly suggestive of hemolysis. Methylmalonic acid and homocysteine levels were significantly elevated to 7890 nmol/L and 71.6 umol/L respectively. She underwent esophagogastroduodenoscopy notable for a single 4cm polypoid, mucosal nodule in the fundus (Figure 1). Antibodies to intrinsic factor and parietal cells were demonstrated, confirming a diagnosis of pernicious anemia. Following transfusion and intramuscular B12 replacement, she was discharged home with ongoing replacement. Biopsy proved chronic active gastritis. The gastric mass was diagnosed as gastric carcinoid and was later resected endoscopically. Two years later she remained on monthly B12 injections, had stable blood counts, showed no signs of tumor regrowth on EGD, and was asymptomatic.
Discussion: As symptoms of pernicious anemia can lead to hospital admission, inpatient physicians should be aware of the disease and its complications. This patient presented with pernicious anemia (PA) and memorable representation of two major complications. PA is an insidious, progressive, autoimmune disease caused by antibodies that decrease production of, or bind and inactivate, intrinsic factor. As intrinsic factor is necessary for the absorption of vitamin B12, patients develop deficiency. B12 plays a role in synthesis of DNA and therefore is crucial for cell proliferation. Amongst the most sensitive to B12 deficiency are the rapidly proliferating hematopoietic precursor cells. As a result, those with PA can develop ineffective erythropoiesis and a resultant megaloblastic anemia. In addition, a small number of patients with PA will develop significant intramedullary hemolysis. This was demonstrated in our patient with a strikingly elevated LDH, unmeasurable haptoglobin, and representative peripheral smear.
This population also has an elevated relative risk of gastric cancer. With decreased acid production from bound parietal cells, uninhibited gastrin secretion can cause rampant proliferation of enterochromaffin-like cells and result in formation of a gastric carcinoid. With this increased risk, it is recommended by the ASGE everyone diagnosed with PA undergo screening endoscopy. This patient presented with a striking anemia with both hemolysis and gastric carcinoid, an unlikely combination of rare complications.
Conclusions: When evaluating a patient with macrocytic anemia with or without hemolysis, one should consider vitamin B12 deficiency. If later diagnosed with pernicious anemia, screening for gastric carcinoid should be conducted.