Background:
Making the hospital discharge process faster and more predictable may help improve patient flow, reduce delays in admitting new patients, and increase hospital capacity. Some hospitals have implemented initiatives to promote timelier discharges as ways to improve hospital throughput. We conducted a national survey of academic medical centers addressing the prevalence, importance, and effectiveness of early discharge initiatives.
Methods:
We assembled a list of hospitalist and general internal medicine leaders representing the 115 prominent academic medical centers belonging to the University HealthSystem Consortium (UHC). UHC is an alliance of non-profit academic medical centers and affiliated hospitals. We then emailed each institutional representative a 30-item online survey regarding early discharge initiatives. The survey included questions about the degree to which early discharge was prioritized at their institution, the prevalence and effectiveness of early discharge initiatives, and barriers to implementation.
Results:
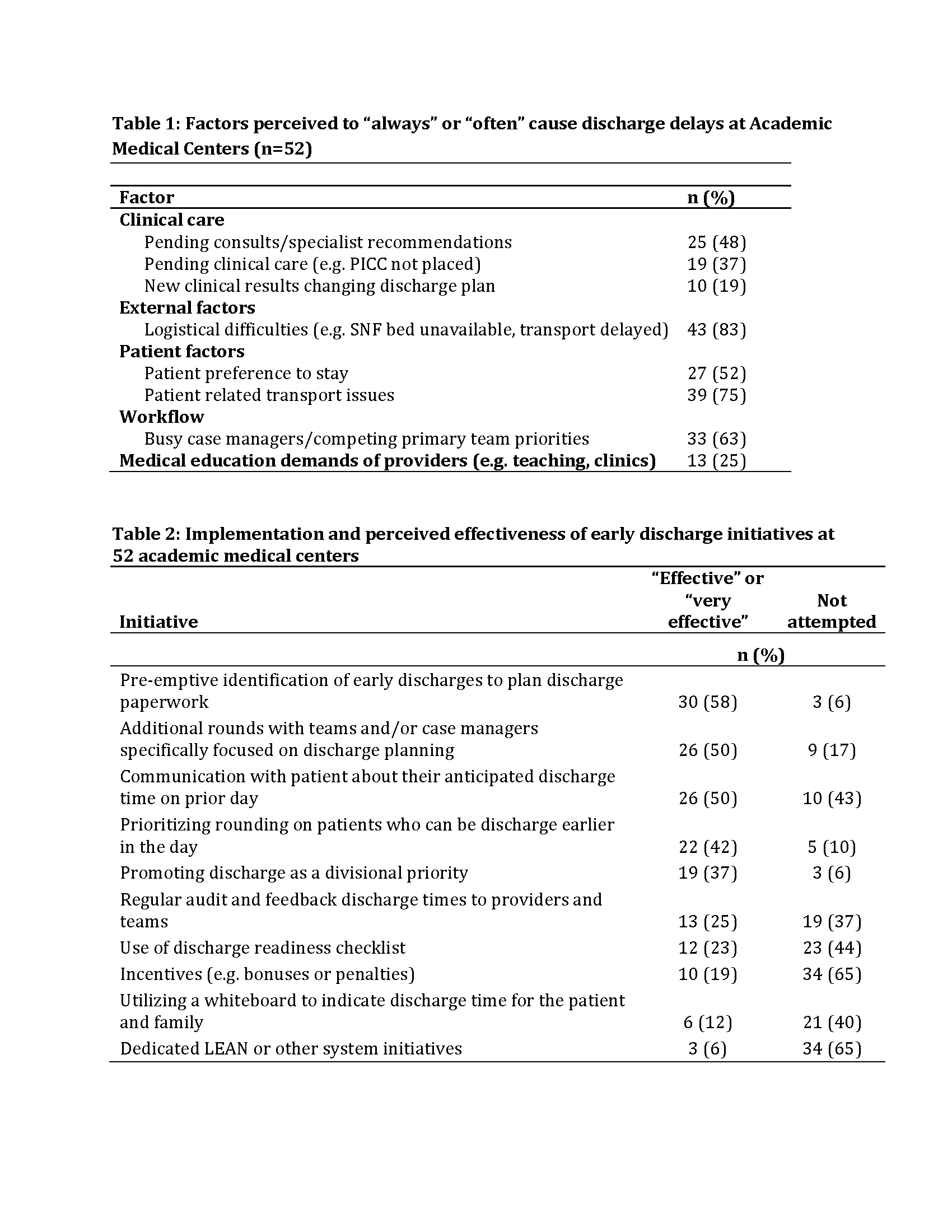
We received 52 responses from the 115 institutions surveyed (45% response rate). Forty-three (83%) ‘strongly agreed’ or ‘agreed’ that early discharge was a priority on their Internal Medicine Service with discharge by noon being the most cited discharge goal (n=20, 38%) followed by 11am (n=11, 21%). The majority of institutions reported discharge by noon to be a more important initiative than obtaining translators for people who do not speak English but as equal importance to reducing 30-day readmissions and improving patient satisfaction. The most commonly reported factors delaying discharge included the availability of post-acute care beds or transport delays for transfers (n=43, 83%), patient-related transport complications (n=39, 74%) or competing priorities of the primary team or case managers (n=33, 63%) (Table 1).
The most effective early discharge initiatives reported by centers involved changes to the rounding process such as pre-emptive identification of patients and early preparation of discharge paperwork (n=30, 58%) and creating discharge planning rounds in addition to daily multi-disciplinary rounds (n=26, 48%) (Table 2).
Conclusions:
Early discharge for medicine patients is a national priority for academic institutions. Institutions have attempted a variety of initiatives to promote earlier discharge but with varying levels of success. Competing priorities and factors external to the hospital were commonly cited impediments to early discharge.