Background: Discharge summaries assist in the transition from inpatient to outpatient care by communicating key diagnoses, medication changes, and follow-up instructions. Despite use of standard formats for discharge summaries through electronic medical records (EMR), primary care physicians (PCPs) report dissatisfaction with locating important information in discharge summaries.
Purpose: The aim of our project was to increase PCP satisfaction with discharge summaries, using satisfaction as a marker for the quality of communication during transitions of care.
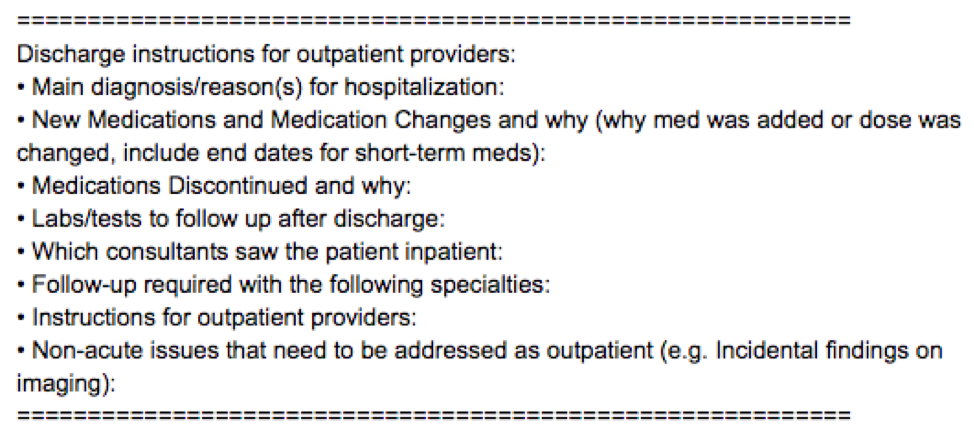
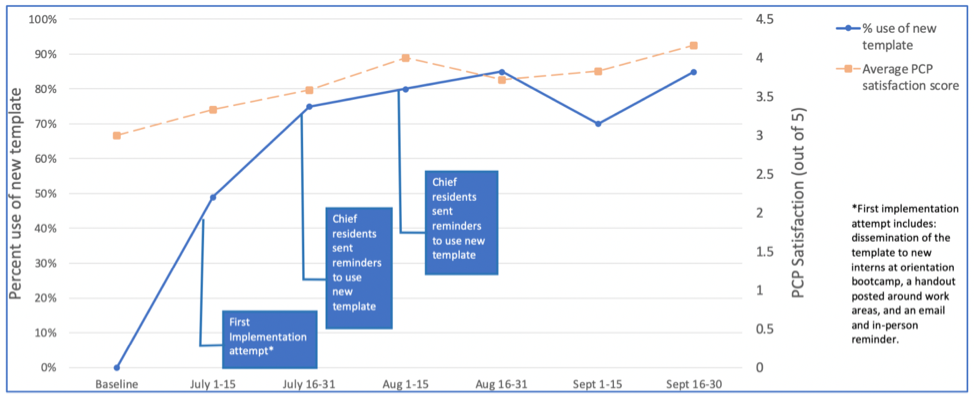
Description: The project was conducted within an internal medicine (IM) residency program at an urban tertiary care academic medical center between 2/2019-10/2019. Causes of suboptimal discharge summaries were determined via focus groups with resident and attending PCPs. Based on the findings, we developed a new template to include in addition to the default discharge summary format in the EMR (figure 1). Our first implementation strategy (week 0) consisted of an outreach campaign through dissemination of the template at intern orientation, a handout, and email and in-person reminders. Residents were reminded about the template by e-mail during weeks 0, 2, and 4 to increase intervention adoption. The project’s outcome measure was PCP satisfaction; the process measure was adoption of new template; and the balancing measure was IM resident barriers to adoption. Every two weeks, random samples of 20 discharge summaries were assessed for template use and 10 were rated by volunteer PCPs for satisfaction (on a 5-point Likert scale with 0=least satisfied to 5=most satisfied). Post-intervention, residents were surveyed regarding their satisfaction and potential barriers to use of the template. Descriptive statistics were used to evaluate trends for all measures. T-test was used to compare average PCP satisfaction with discharge summaries with and without the new template. A total of 1,184 discharge summaries were completed on two IM floors over three months; 120 summaries were sampled to assess for new template use, and 60 summaries were rated by PCPs. Comparing measures at baseline to after three implementation cycles, PCP satisfaction increased from an average score of 3.0 (out of 5) to 4.1 and new template adoption increased from 0% to 85% (figure 2). The mean PCP satisfaction rating of discharge summaries was 4.1 with and 3.6 without the new template (p=0.10). Thirty residents out of 74 responded to the post-intervention survey (41% response rate) and reported that it was not more difficult to use the new template (90%) and not more time consuming (55%). Residents thought that discharge summary quality improved with the incorporation of the template (93%) and would like the template to be a part of the default discharge summary template in the EMR (93%).
Conclusions: Creating a discharge summary template to target PCP-identified high-yield information resulted in a trend of increased PCP satisfaction with high rates of adoption by IM residents. Next steps include continuous improvements to the template and incorporating these changes into the default discharge summary. This resident-led quality improvement project may be used as a model for other institutions to engage trainees in QI initiatives.