Background: Alcohol use disorder (AUD) is a pervasive disease affecting 28.6 million (11.3%) American adults in 2021.1 Medications for AUD (MAUD), including naltrexone, acamprosate, and disulfiram, are effective, yet less than 5% of these patients received treatment.1,2 Inpatient encounters of patients with AUD present a crucial opportunity to initiate MAUD, prompting this quality improvement (QI) project.3 Our overarching goal is to enhance MAUD prescribing rates among hospitalized patients with AUD. As a first step, we explored treatment disparities within our prescribing practices and identified improvement opportunities to provide long-term benefits for patients with AUD.
Methods: Our project is being conducted at a quaternary medical center, encompassing data from three main hospitals across three states. Utilizing the DMAIC framework for QI, we focused on the measurement and analysis phases to examine treatment disparities among patients with AUD. We obtained data on MAUD prescriptions, patient demographics, and encounter details for adults with an AUD-related diagnosis who sought emergency services or were hospitalized between 2018 through 2023. In our analysis, we compared MAUD prescription rates among patients according to dichotomous rational subgroups using Chi-square analysis, with a significance level set at 0.05. Patients excluded from the analysis were those with MAUD prescriptions continued from prior, discontinued, or changed during the encounter.
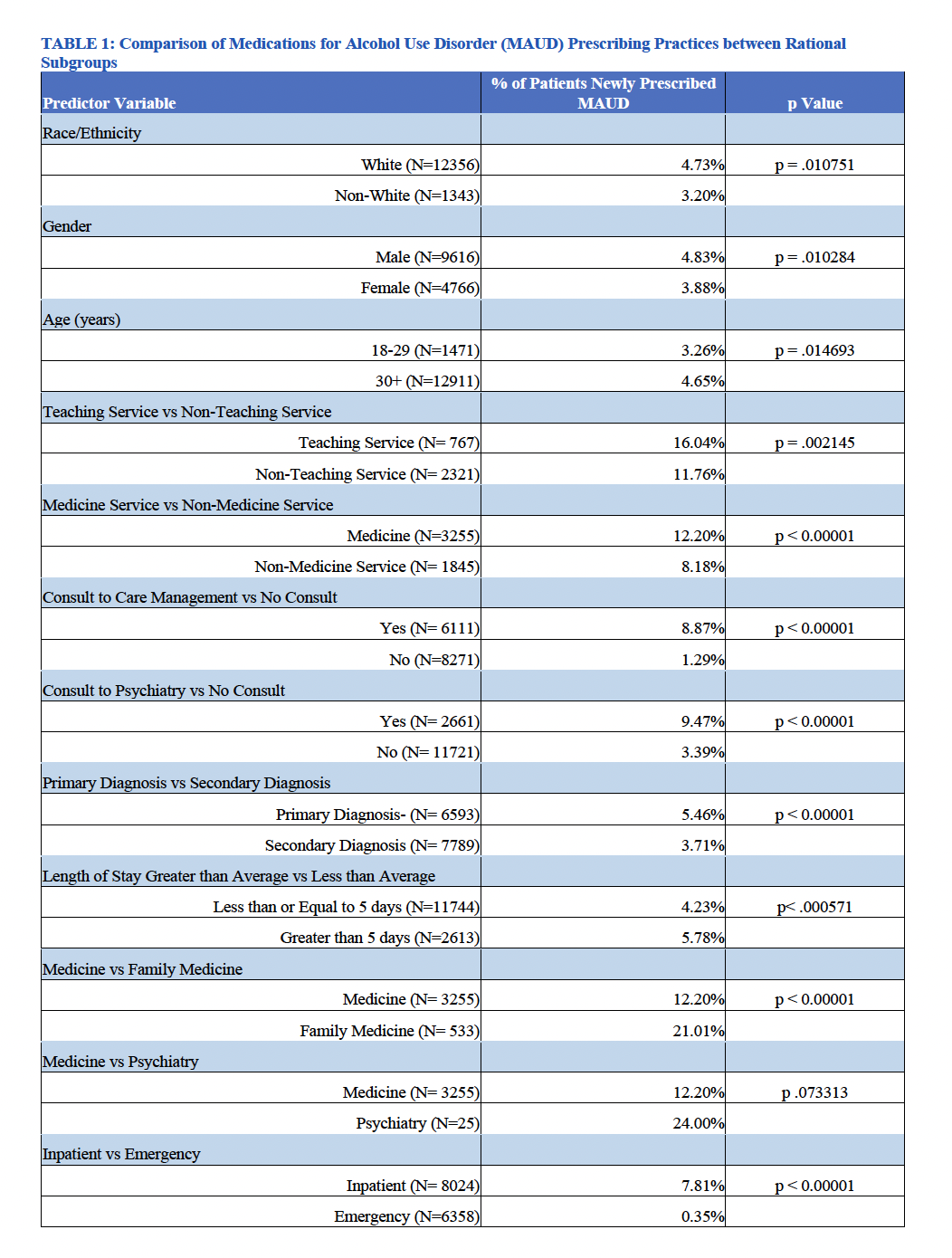
Results: We analyzed 14,870 hospitalizations in which AUD was either a primary or secondary diagnosis, involving over 8,000 distinct patients. From this cohort, 649 (4.36%) patients were newly prescribed MAUD during the encounter, 488 (3.28%) already had a prescription prior to the encounter, and 13,733 (92.35%) were not prescribed any MAUD. Patients had significantly higher rates of MAUD prescription if they were: white (vs. non-white), male (vs. female), age 30 + (vs. 18-29), on a teaching service (vs. non-teaching service), on a medicine service (vs. non-medicine service), had either a consult placed to psychiatry or care management (vs. no consult placed), primary diagnosis of AUD (vs. secondary diagnosis), length of stay >5 days (vs. 5 days or less), on a family medicine service (vs. medicine service), and inpatient admission (vs. emergency department visit) [Table 1].
Conclusions: We urgently need to enhance our treatment practices for patients with AUD in the hospital. We have identified disparities in MAUD prescribing rates within specific patient demographics and hospitalization characteristics. These results highlight the importance of rational subgrouping, which will inform our development of future tailored improvement efforts with the goal of increasing our MAUD prescribing rates.