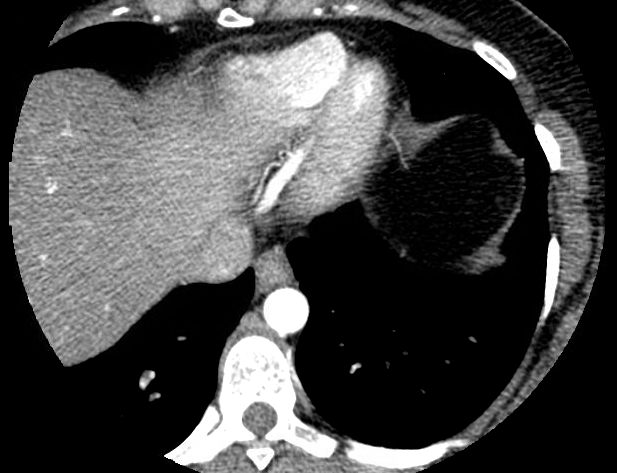
Case Presentation: A 32 year old female presented with 2 month history of acute onset pressure-like chest pain occurring after yelling at her children and radiating to the back. The symptoms recurred and become progressive while doing house chores. The pain was relieved by rest. Family history was positive for premature coronary artery disease, dyslipidemia and hereditary hemorrhagic telangiectasia. Examination revealed severe hypertension but no significant difference when taken from both arms. Laboratory data revealed negative troponin and ECG was without acute ischemic changes. Lipid profile showed elevated cholesterol. CT chest was unremarkable, however Coronary angiography CT showed tapering of the mid to distal left anterior descending coronary artery territory suggestive of coronary dissection. The coronary artery calcium score was 0.
She was managed with beta blockers, nitrates, Ranolazine, dual antiplatelet therapy and statins with good clinical outcome.
Discussion: Spontaneous coronary artery dissection (SCAD) is defined as a non-traumatic and non-iatrogenic separation of the coronary artery walls, creating a false lumen and intramural hematomas leading to decreased blood flow and myocardial ischemia . It is an uncommon and poorly understood cause of acute coronary syndrome (ACS), myocardial infarction and sudden cardiac death. SCAD is a rare cause of acute coronary syndrome with incidence of 0.04% to 0.2% of coronary angiographies. It is associated with sudden death in 50% of cases. 75% of affected patients are female, with an average age 40 years old at the time of diagnosis.
Predisposing risk factors include fibromuscular dysplasia, pregnancy, connective tissue diseases, cystic medial necrosis, hypertension, hormone replacement therapy, strenuous exercise, vasospasm, cocaine and tobacco use. Typically patients are young and do not exhibit the classic risk factors for coronary artery disease as seen in our index case.
The exact incidence, prevalence, etiology, prognosis, recurrence rate, and best management of SCAD remain unclear, but increasing awareness has led to early detection and new insight into this rare disease entity. The clinical presentation is variable with chest pain being the most common presenting symptom. Ventricular arrhythmia occurred in 8%-14% of patients, troponin elevation and ST-segment elevation in 26%.
Coronary angiography allows for early diagnosis of SDCA. More than 80% of acute SCAD patients are treated medically with standard medical therapy as in ACS. Only 3.3% require revascularization. Our patient had a good clinical outcome on medical treatment alone.
Conclusions: In conclusion, SCAD should be considered in every young patient presenting with chest pain even in the absence of troponinemia or significant EKG findings. Conservative treatment continues to be the first line in management of young people without ominous signs.