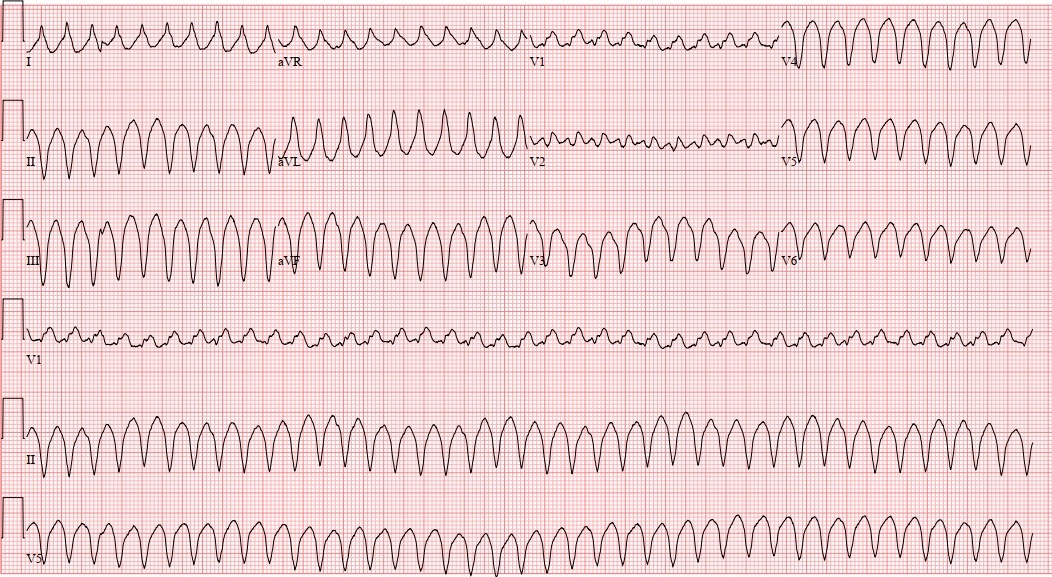
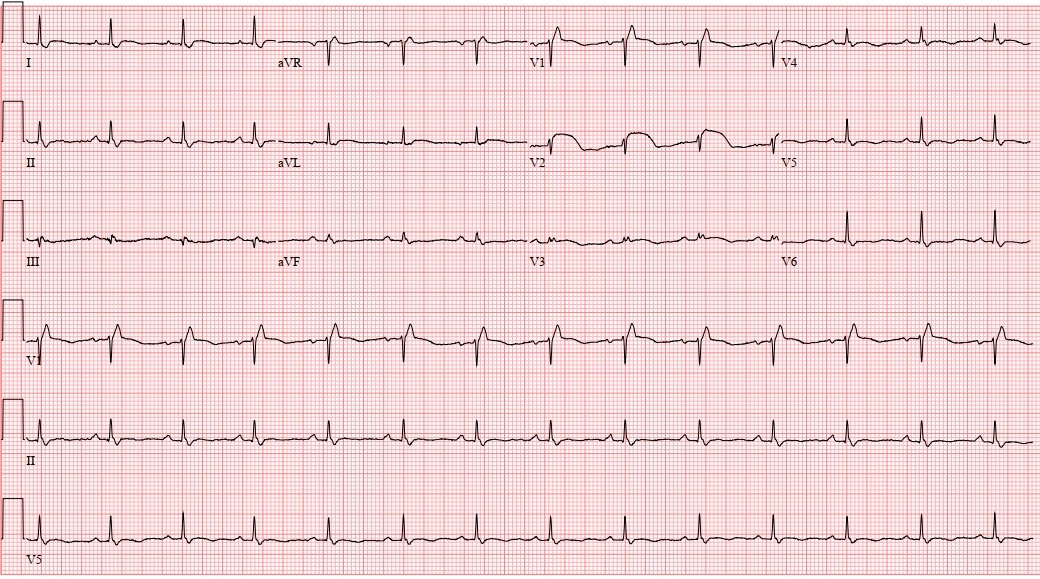
Case Presentation: 36-year-old female with no past medical history presents with vomiting and abdominal pain after eating a meal. Symptoms were accompanied by diaphoresis, dizziness, and palpitations. On arrival to the hospital, patient’s vital signs were stable. Labs were significant for WBC 11 K/cumm, AST 64 U/L, ALT 47 U/L. Computed tomography of the abdomen/pelvis showed steatohepatitis. She was given IV ondansetron 4mg and IV prochlorperazine 5mg in addition to 1 liter of IV fluids, then she was admitted for observation. Overnight, patient had a sudden recurrence of presenting symptoms. On exam, she appeared acutely distressed, dyspneic, and diaphoretic. Patient was tachypneic to 36 breaths per minute, hypotensive to 80/50, with a heart rate that was difficult to pick up on the monitor. Stat EKG showed monomorphic ventricular tachycardia at 240 bpm (Figure 1). Patient underwent synchronized cardioversion at 150 joules with resolution of unstable VT. Once stabilized, repeat EKG showed findings consistent with Type 1 Brugada pattern (Figure 2). Upon further chart review, a prior EKG years ago had also shown Type 1 Brugada pattern. Patient ultimately had an implantable cardiac defibrillator placed for secondary prevention.
Discussion: Brugada syndrome is a rare inherited channelopathy disorder that predisposes patients to ventricular tachyarrhythmias and sudden cardiac arrest. On EKG, Brugada pattern is characterized by pseudo-right bundle branch block and ST-segment elevation in leads V1 and/or V2. Type 1 Brugada pattern has a “coved pattern” with a ≥2mm elevated ST segment that descends into an inverted T wave. Type 2 Brugada pattern has a “saddle back pattern” with an elevated ST segment which descends then ascends again into a T wave. Brugada syndrome is diagnosed when the Brugada pattern is accompanied by either ventricular tachyarrhythmia or sudden cardiac death. Triggers that can induce Brugada pattern include fevers, medications (such as sodium channel blockers), alcohol or other toxins, and electrolyte disturbances. Diagnosis of Brugrada syndrome requires exclusion of structural heart disease and alternative diagnoses. In patients who have type 2 Brugada pattern or an uncertain diagnosis, a procainamide challenge can be performed. The drug challenge is positive if type 1 Brugada pattern is elicited. Management of Brugada syndrome involves avoiding known triggers. Implantable cardiac defibrillators are placed in any patients who have history of cardiac arrest or sustained VT. Other high-risk patients including those with syncope are also considered for ICD placement. Alternative therapies include anti-arrhythmic medications and VT ablation. Relatives should be screened for clinical features and EKG patterns, but there is limited data on routine genetic or electrophysiological testing of first-degree relatives.
Conclusions: It is important not to anchor on the first obvious diagnosis. In a young, healthy patient it is easy to dismiss this case as food poisoning. In retrospect, the patient’s initial presentation was likely a clinical manifestation of ventricular tachycardia. A more thorough chart review would have revealed that the patient had a prior history of Brugada pattern. Additionally, an EKG was not performed on admission, which should have been a consideration in the setting of certain red flag symptoms and administration of QT-prolonging IV anti-emetics. Fortunately, this patient was able to receive the appropriate diagnostic work-up and treatment.