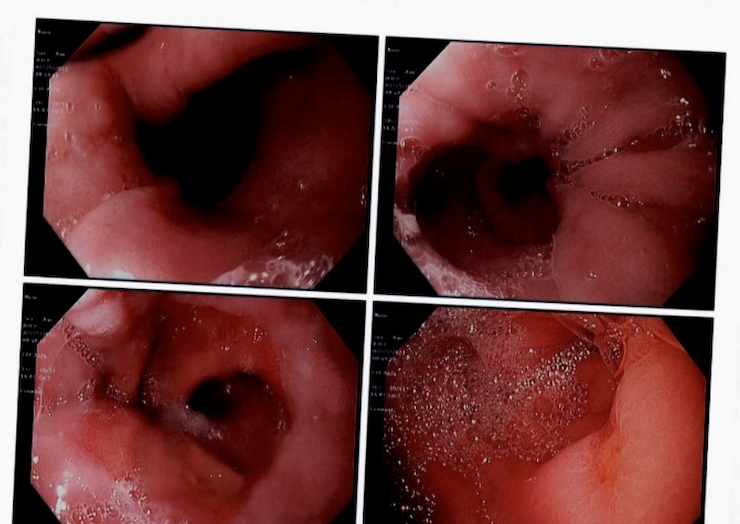
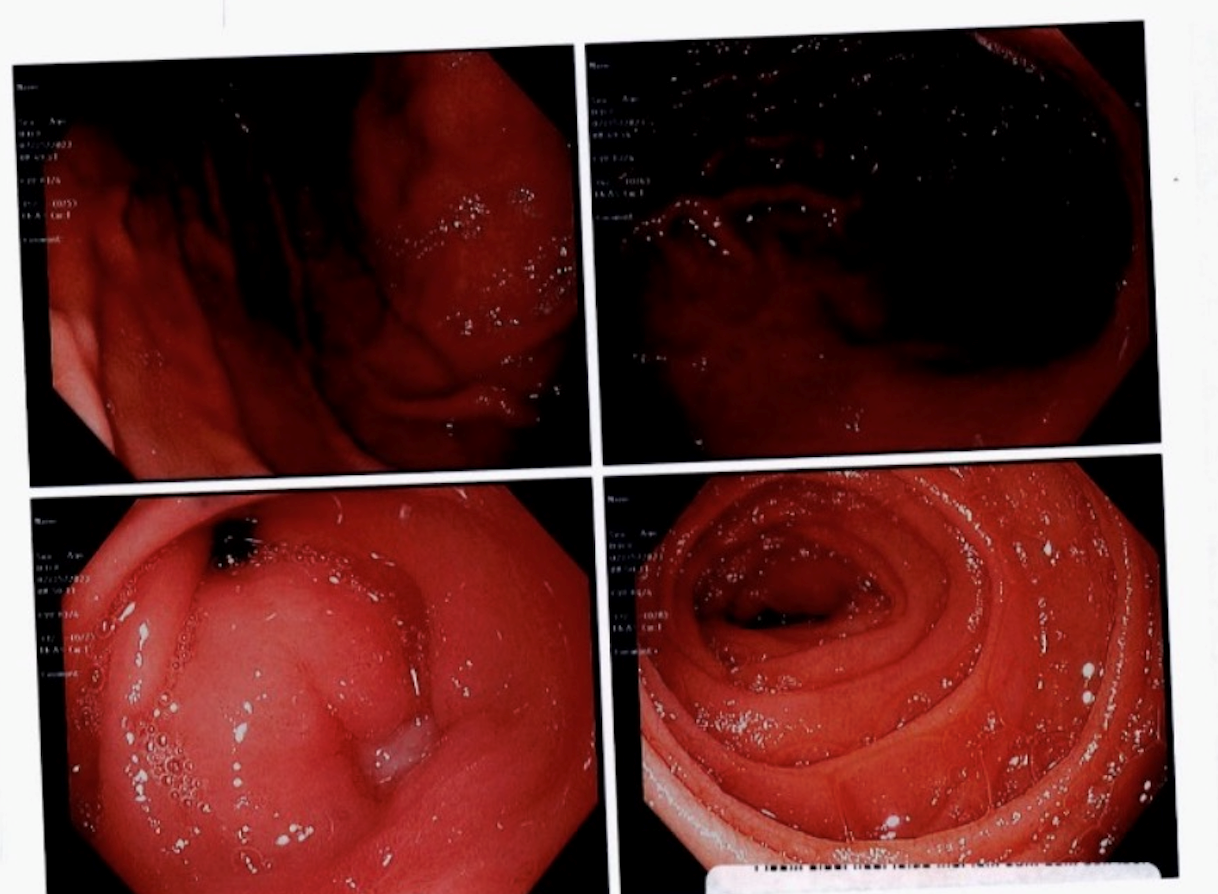
Case Presentation: A 67-year-old male with a history of Graves’ disease, paroxysmal atrial fibrillation status post cardiac ablation not on anticoagulation, and chronic ibuprofen use presented to the emergency department with progressive dizziness, fatigue. He noted 10 days of black stools. Additionally, patient’s wife reported he had confusion that started yesterday. Patient presented stable on room air with stable blood pressure of 144/61 mmHg and heart rate of 111 bpm. Physical examination was notable for asymmetric goiter, exophthalmos, and nontender abdomen. Hemoglobin was 7 g/dL. Given the patient’s chronic NSAID use, an acute UGIB was suspected. Gastroenterology was consulted and the patient was scheduled for upper endoscopy (EGD) the next morning.Routine thyroid function test results came back 3 hours prior to scheduled EGD, which revealed elevated free T4 at 3.05 ng/dL and undetectable Thyroid stimulating hormone (TSH), < 0.005 mIU/L. Calculation of the Burch-Wartofsky Point Scale for Thyrotoxicosis resulted in a score of 45, which is highly suggestive of thyroid storm. Gastroenterology was contacted to cancel the scheduled endoscopy. Endocrinology was consulted. Treatment was initiated with methimazole, propranolol, and hydrocortisone. His mental status was back to baseline on the second day of hospitalization. He required 5 units of packed red blood cells in the first 3 days of hospitalization due to persistent melena. Computed tomography angiography of the abdomen/pelvis showed no evidence for active bleed on day 3 of the hospital course. Free T4 had improved from 3.05 to 2.32 ng/dL in this time period. Once the patient's tachycardia had stabilized and improvement was noted in TSH and T4 levels, it was deemed safe to proceed with the procedure. The upper endoscopy was performed on the fifth day of hospitalization, which revealed two 8-mm nonbleeding ulcers in the prepyloric antral region. The patient was subsequently discharged on pantoprazole, sucralfate, methimazole, and propranolol
Discussion: Thyroid storm, a rare, life-threatening constellation of acute hypermetabolic effects, is a feared complication of chronic hyperthyroidism. Patients undergoing general anesthesia have particularly elevated mortality in acute thyroid storm due to the rapid increase in end-organ oxygen requirements from metabolic augmentation.[1] There is a notable lack of definitive evidence and consensus on guidelines for perioperative management of these patients.[2] Because of these serious risks of complications and the inability to predict which patients are more likely to experience them, it is still recommended that hyperthyroid patients receive preoperative treatment.[3]
Conclusions: This case illustrates the complex challenge of two unrelated, acute pathologies, each complicating management of the other. Treatment of thyroid storm requires high-dose steroids, and the need for general anesthesia for the suspected UGIB created a therapeutic dilemma, as corticosteroid use in hospitalized patients is associated with increased risks of gastrointestinal bleeding.[4] Each intervention elevated the risks associated with the other condition. The decision was made to cancel EGD due to the threat of end-organ ischemia from anesthesia-induced vasodilation in the setting of thyroid storm.[3] Owing to the coordinated efforts of the endocrine and gastroenterology teams, this patient’s dual pathologies were effectively managed, resulting in a positive outcome to a high-risk scenario.