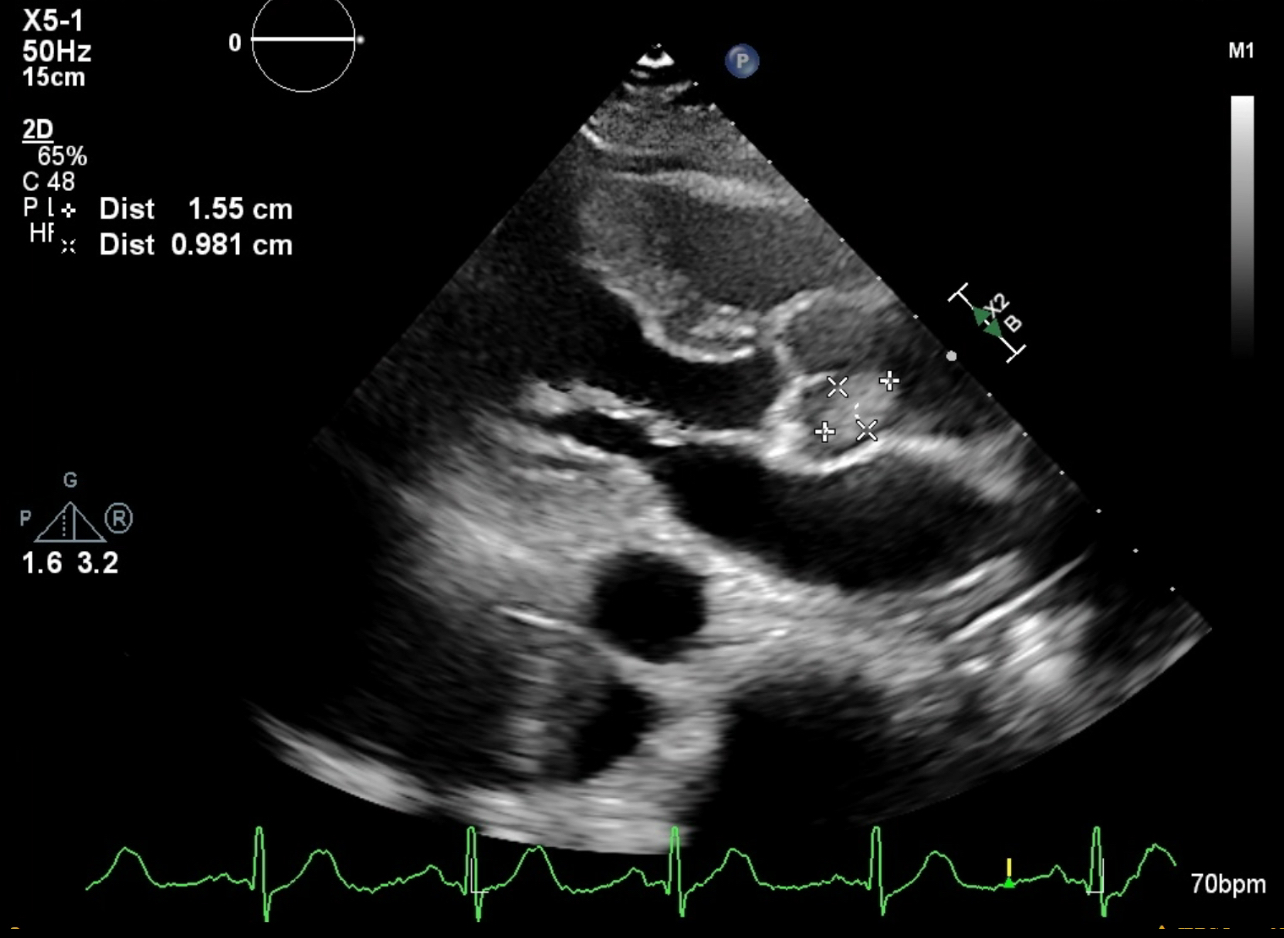
Case Presentation: A 73-year-old woman with past medical history of hypertension was discovered unresponsive at home, prompting initiation of CPR during transportation to the Emergency Department, resulting in the restoration of spontaneous circulation (ROSC). A chest x-ray indicated the presence of left-sided tension pneumothorax, necessitating the placement of a chest tube. Initial electrocardiogram (EKG) findings revealed acute ST segment elevations in the inferior leads ll, lll, aVF. Urgent cardiac catheterization disclosed no evidence of coronary artery disease or acute culprit lesions. Transthoracic echocardiogram (TTE) demonstrated a normal ejection fraction (EF) of 60-65% with moderate aortic valve sclerosis. The patient’s intensive care unit (ICU) stay was complicated by seven instances of cardiac arrest, each successfully managed with resuscitation. Subsequent TTE identified a 1.5 x 0.9 cm echogenic mass in anterior coronary cusp of the aortic valve, associated with a diminished EF of 20-25% and severe wall motion abnormalities. Attempts to conduct a transesophageal echocardiogram (TEE) were thwarted by constriction of the upper esophageal sphincter. Consequently, the patient underwent emergent resection of the aortic valve mass, coupled with aortic valve repair. Pathological examination confirmed the diagnosis of cardiac papillary fibroelastoma. Post-surgery, a follow-up TTE demonstrated an improved EF of more than 60%, a competent aortic valve, and no evidence of any mass. The patient was discharged to an inpatient rehabilitation facility with scheduled follow-ups with cardiothoracic surgery.
Discussion: Primary cardiac tumors are uncommon, occurring in less than 0.03% of cases, with Cardiac Papillary Fibroelastoma (CPFE) ranking as the second most prevalent tumor following myxoma. Of CPFE cases, over 70% are benign, with papillary fibroelastomas accounting for only 8%. These benign primary neoplasms of the heart often exhibit no symptoms and are typically discovered incidentally. However, they can lead to significant complications, such as ventricular fibrillation, stroke (most commonly observed), myocardial infarction, and sudden death (2). Prompt diagnosis is crucial, starting with transthoracic echocardiography (TTE) as the initial step, followed by transesophageal echocardiography (TEE) for enhanced mass visualization, and confirmation through histologic examination.While PFEs can be found on any heart valve, the aortic valve is the most frequent site (35-63%). The recommended course of action involves surgical excision and repair of any associated cardiac defects. Given the benign nature of PFEs, the prognosis is generally favorable after the removal of the mass. In cases where surgery is not a viable option or if the patient is asymptomatic, anticoagulation coupled with vigilant monitoring for potential cardioembolic events may be a reasonable alternative (1).
Conclusions: In conclusion, this case underscores the complexity of cardiac papillary fibroelastomas (CPFE), highlighting the diagnostic challenges and life-threatening potential. The successful emergent resection and aortic valve repair demonstrated the critical role of prompt intervention. Postoperatively, notable improvements in echocardiographic parameters reinforce the efficacy of surgical management. This case emphasizes the importance of a multidisciplinary approach and vigilant postoperative surveillance in effectively managing CPFE.