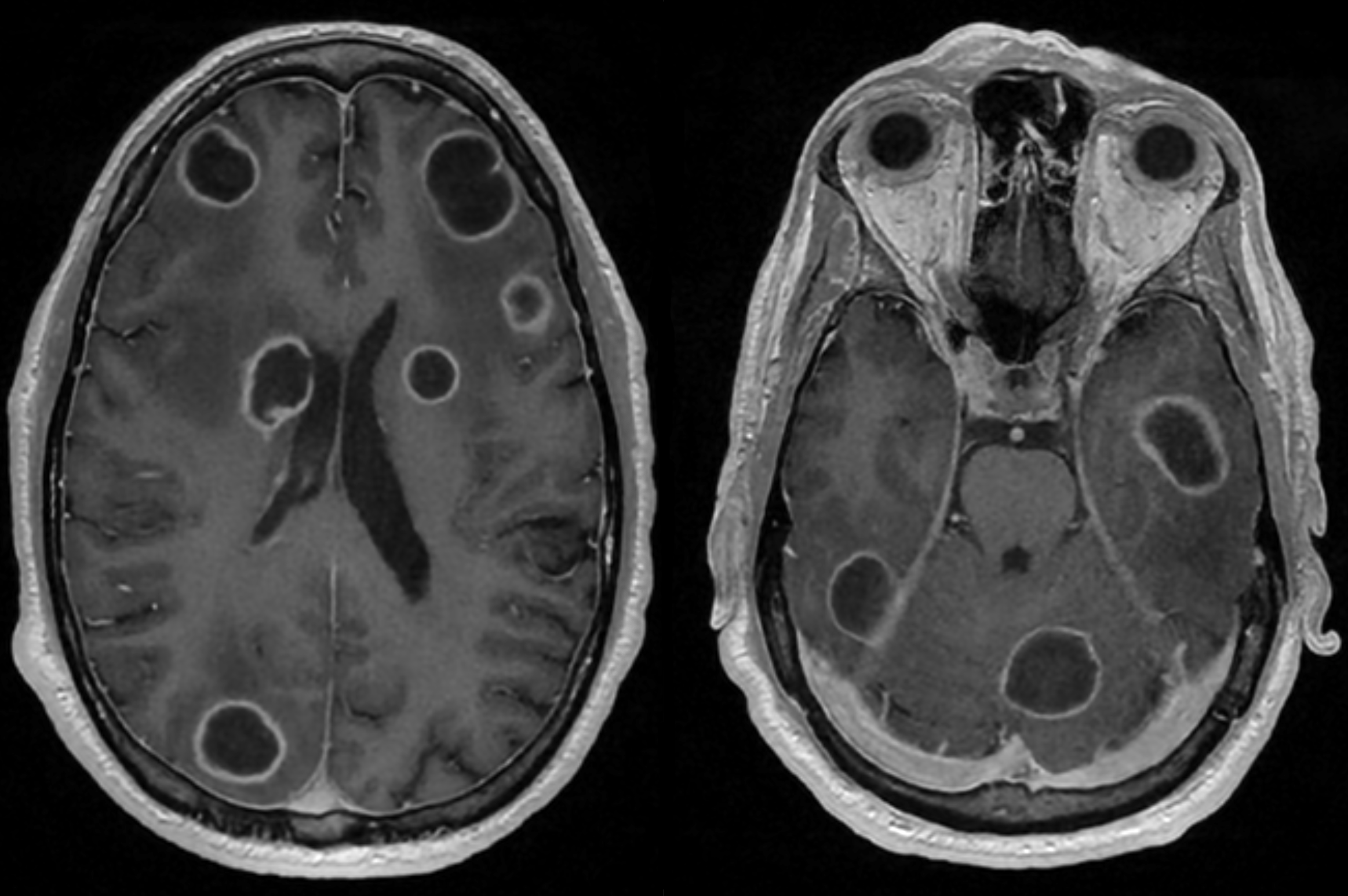
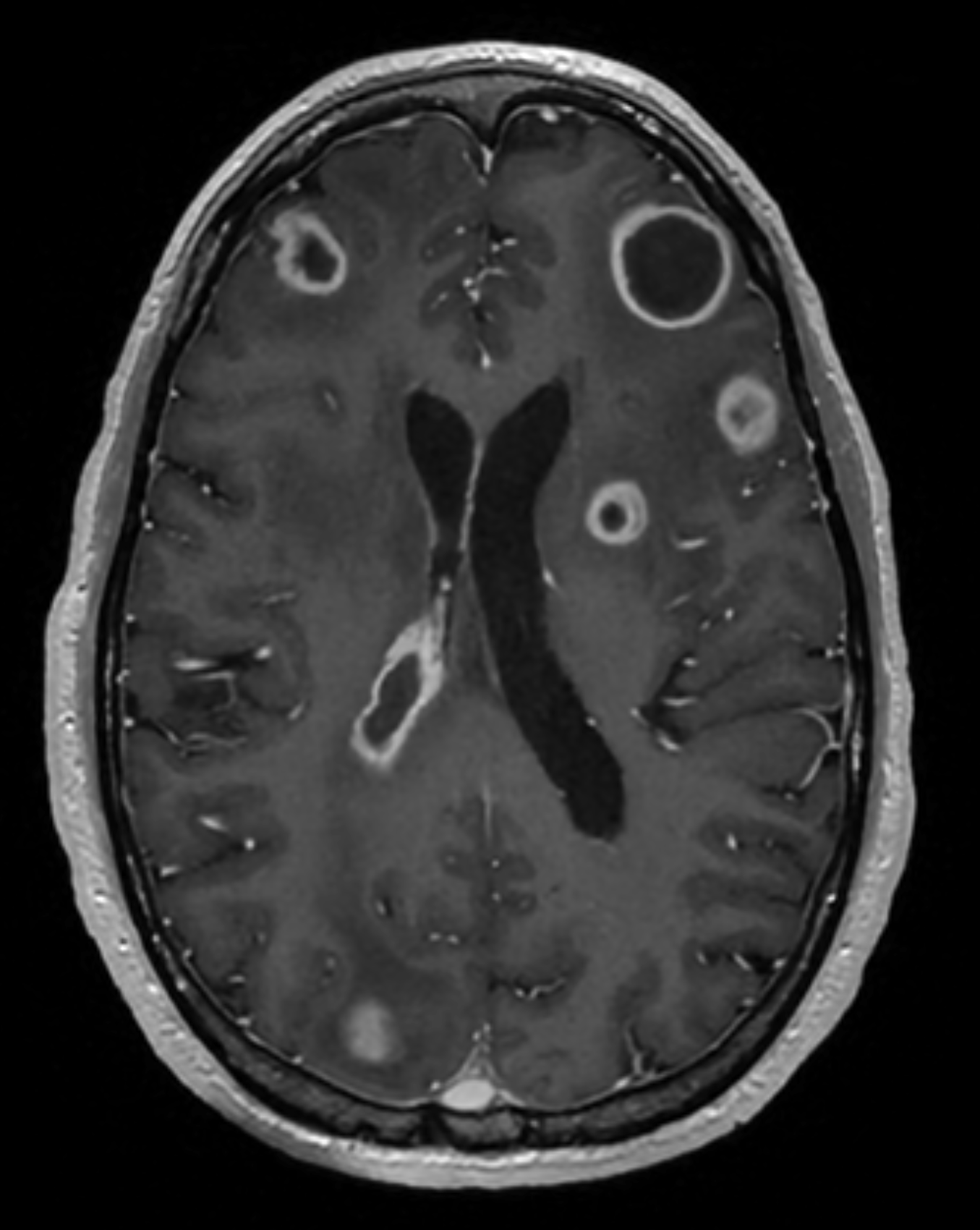
Case Presentation: A 56-year-old immunocompetent man with history of inhaled methamphetamine use, poor dentition and recent all-terrain vehicle (ATV) accident requiring chest tube, presented with 1 week of progressive hallucinations, who was found to have multiple ring enhancing brain lesions. Initially, he was afebrile with normal vitals, minimally responsive to noxious stimuli and moving all extremities. WBC was 25.6 k/uL and CRP 94 mg/L. Peripheral blood cultures, HIV, RPR, quantiferon, and fungal studies were negative. Brain MRI revealed extensive vasogenic edema and multiple ring enhancing lesions consistent with brain abscesses (Image 1). CT chest showed stable mediastinal mass from the time of the ATV accident. Culture obtained via burr hole aspiration grew Streptococcus intermedius. Dexamethasone, levetiracetam, and 6 weeks of ceftriaxone and metronidazole were started. By hospital day 10, mental status improved and he returned home. A month later, after elective tooth extraction, he was readmitted to the hospital for encephalopathy and headache. He was afebrile with mild leukocytosis and repeat MRI brain showed interval decrease in size of all intracranial abscesses and new ventriculitis from ruptured abscesses (Image 2). Antibiotics were continued and his ventriculitis-associated headaches improved with gabapentin, nortriptyline, and acetaminophen.
Discussion: The differential diagnosis for multiple ring enhancing brain lesions is dependent on immune status. In immunocompromised hosts, infectious etiologies (e.g toxoplasmosis and endemic mycoses) and primary central nervous system lymphoma are most prevalent. In immunocompetent hosts, the diagnosis favors malignancy but pyogenic abscesses or demyelinating diseases may be present. Tuberculomas and parasitic infections should be considered in both groups. Definitive diagnosis is made via brain biopsy, but comes with considerable risk. Therefore, discussion with radiology is encouraged as radiologic features can help elucidate the etiology. We recommend close attention to T-2 weighted sequences on MRI and consideration of alternative modalities, such as MR spectroscopy or PET, to evaluate lesion metabolism if biopsy is unable to be obtained.In this case, streptococcus intermedius was identified as the causal organism. Common sources include local (e.g. dental, sinus, ear) versus hematogenously (e.g. liver) spread infections. While the primary source remains unclear, the patient notably had poor dentition, recent severe trauma, and mediastinal mass. Repeat chest imaging, showed reduction in mass size after 5 days of antibiotics, suggesting an infectious etiology possibly due to ATV accident.The patient’s readmission with persistent leukocytosis, altered mental status and headaches were sequelae from original abscesses and likely unrelated to the dentition. In cases of recurrent neurologic symptoms, we recommend repeat imaging to identify complications (e.g. ventriculitis), confirm stability or reduction in abscess size, and possibly identify an incorrect diagnosis or secondary underlying process.
Conclusions: Multiple Streptococcus intermedius brain abscesses in immunocompetent individuals without injection drug use is exceedingly rare. This should prompt assessment for local or hematogenous sources of infection. Management of brain abscess includes antibiotics, consideration of biopsy or aspiration for source control, definitive diagnosis, and treatment of ventriculitis-associated headaches.