Background: Prescribing of opioid medications has been a hot button issue for at least a decade now. Hospitalists play a unique role as we are on the front lines of patient care and have to coordinate care between specialists and primary care physicians. That role as well as patient demands may make the path of least resistance a prescription for opiate medications. With the volume of patients as high as it is, individual hospitalists may have very little idea about the number of prescriptions they write each month.
Purpose: Awareness of real-time individualized discharge opioid prescribing practices has not previously been readily available to hospitalists. We hypothesized that providing access to this information would reduce opioid prescription rates at discharge. The objective of this study was to compare opioid prescription rates of hospitalists before and after receiving this feedback.
Description: A descriptive study was performed on 15 hospitalists’ opioid prescription rates. Opioid prescription rates were obtained from the electronic medical record by a single unblinded abstractor previously employed as a data engineer for this EMR. Discharge opioids were defined as prescriptions written for buprenorphine, butorphanol, codeine, dihydrocodeine, fentanyl, hydrocodone, hydromorphone, levorphanol, meperidine, methadone, morphine, oxycodone, oxymorphone, pentazocine, tapentadol, and tramadol. The hospitalists received an insight about their prescribing habits in a text message, which compared their rate with their peers in a bar graph. The percentage of opioid prescriptions per discharged patient for individual hospitalists and the cohort was compared 60 days before to 60 days after the insight was sent.
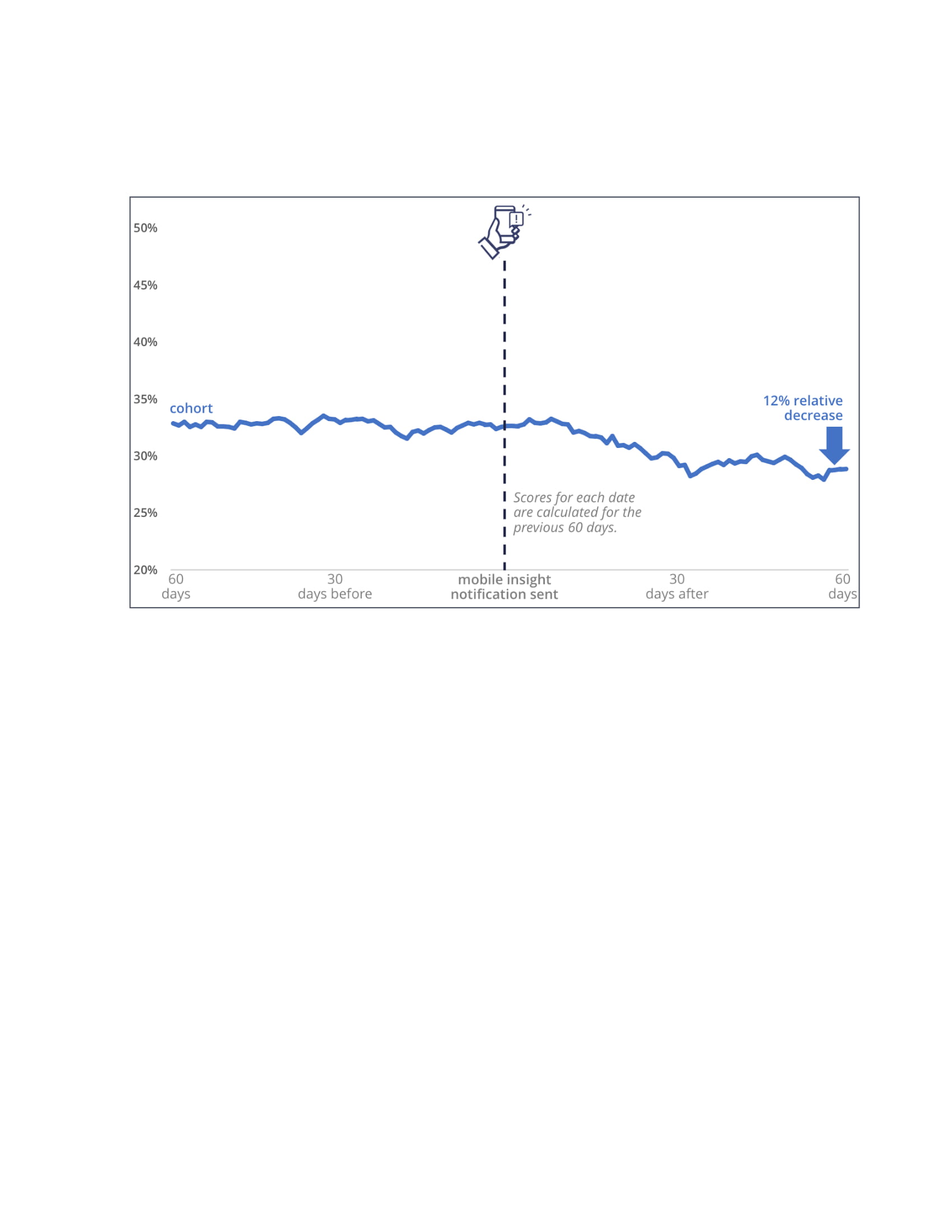
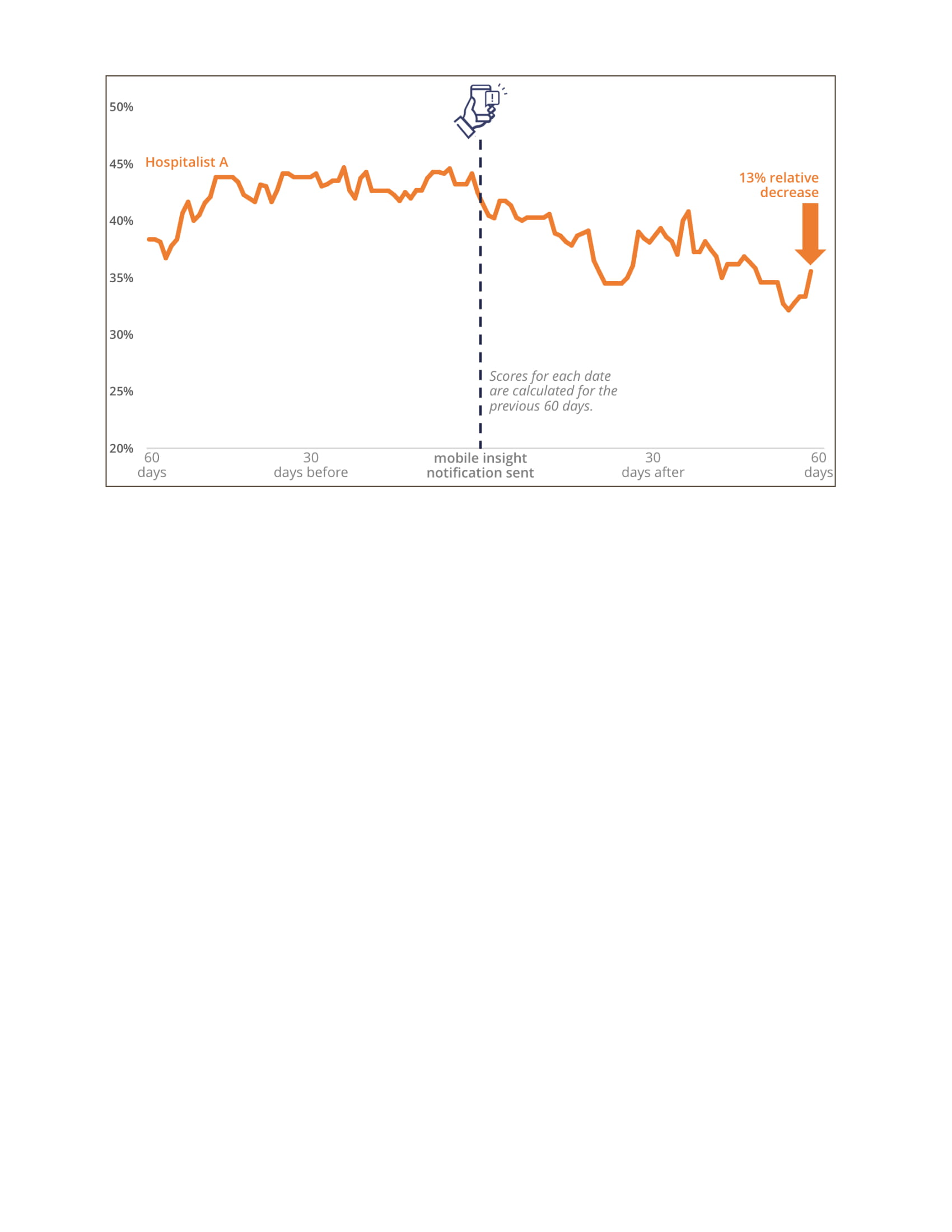
Conclusions: During the 60-day period prior to the text notification, the group’s average opioid prescription rate was 32.7%, compared to 28.9% afterwards, a 12% absolute decrease.(Figure 1) Hospitalist A, who had the highest baseline prescription rate in the cohort, demonstrated a 13% reduction in their prescription rate. (Figure 2) While neither this nor the group rate were significant changes, the prescription rates are continuing to decline after the 60-day window, suggesting a trend towards significance.
Mobile-enabled, real-time, transparent, individualized feedback is a powerful tool for building awareness of individual practice habits, including opioid prescribing rates at discharge. Such platforms have the potential to influence clinical decisions and surface opportunities for behavior change in opioid prescribing. Further studies are needed to determine the cost-benefit and the long-term effects of these solutions.