Case Presentation: A 56 y/o African American male with a history of paroxysmal atrial fibrillation presented with “pounding” chest pain after being assaulted. On presentation, the patient was afebrile and normotensive but significantly tachycardic (heart rate 140). Physical exam revealed an irregular rhythm with a s3 gallop and a 2/6 systolic murmur in the left sternal border that worsened with Valsalva. Chemistries, complete blood counts, and thyroid function tests were within normal limits. BNP (409 ng/dL) and troponins (0.05ng/mL) were mildly elevated. Urine drug screen was negative.
Electrocardiogram revealed a bifascicular block and a tachycardic heart rate of 140 beats per minute (bpm) concerning for supraventricular vs sinus tachycardia vs atrial fibrillation/flutter. The patient was loaded with adenosine 12mg which revealed atrial flutter, with subsequent direct current cardioversion into normal sinus rhythm. Beta blockers were initiated, however, the patient continued to have frequent runs of symptomatic, non-sustained ventricular tachycardia.
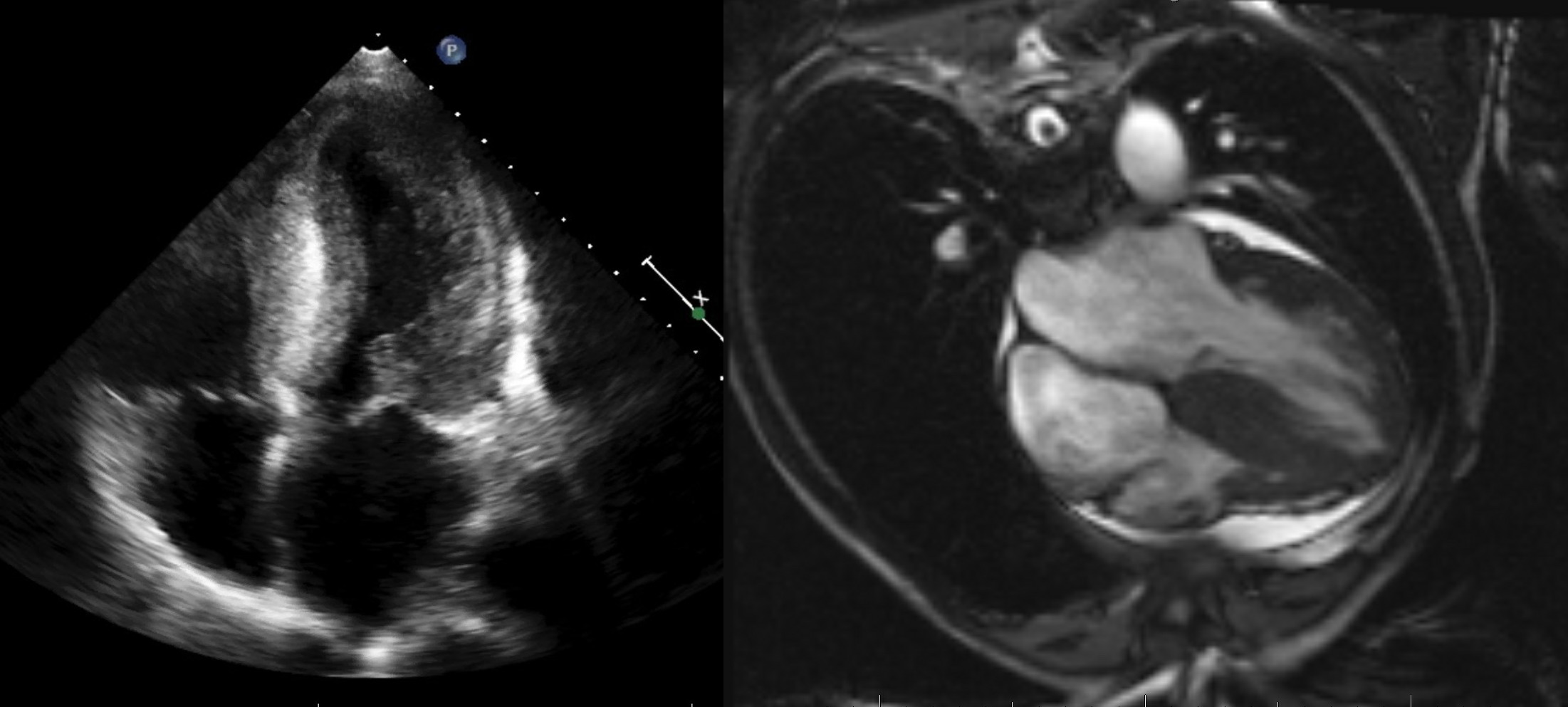
Transthoracic Echocardiogram (ECHO) revealed a small left ventricular cavity, severe asymmetric left ventricular hypertrophy (LVH), systolic anterior motion (SAM) of the mitral valve, and a left ventricular outflow tract (LVOT) gradient, all consistent with hypertrophic obstructive cardiomyopathy (HOCM). Exercise stress ECHO 2 days later noted left ventricular cavity obliteration but improvement in the initial LVOT gradient. Cardiac MRI revealed asymmetric hypertrophy of the anterior septal (30mm) and inferior left ventricular walls with evidence of delayed gadolinium enhancement indicative of scar or fibrosis. Automated implantable cardioverter defibrillator (AICD) was placed after extensive discussion with the patient and his wife given his high risk of sudden cardiac death (SCD). Beta blockers were uptitrated to a target heart rate of ~65 bpm and he was discharged in stable condition with instructions to avoid strenuous physical activity. On follow up visits, the patient remained asymptomatic.
Discussion: Hypertrophic cardiomyopathy (HCM) is a genetic cardiac disease characterized by ventricular wall hypertrophy in the absence of any other conditions causing cardiac overload. HCM typically has a relatively benign course but is a leading cause of sudden cardiac death (SCD) due to ventricular tachyarrhythmias, especially in young adults who experience obstructive physiology. Although SCD is more common in the younger population, the current risk prediction model is inadequate and cannot accurately identify individuals who may experience SCD. However, patients with increasing age appear to have a more benign clinical presentation with a lower risk of symptoms and SCD. Even so, findings such as severe LVH, LVOT obstruction, and late gadolinium enhancement can lead to deleterious effects on myocardial architecture and myocardial oxygen demand, resulting in unpredictable disease progression. For these high risk patients, a thorough discussion of the risks and benefits of AICD placement should be held to allow for active patient participation in the decision making process.
Conclusions: HOCM is a leading cause of SCD, especially in young adults, but can lead to symptoms at any age. Given the concern for SCD, physicians must identify and educate high risk HOCM patients with obstructive features at any age to advocate for AICD placement to prevent, and abort, life threatening tachyarrhythmias.