Background: Lung transplant recipients are a unique cohort of patients who require a multidisciplinary approach to management when hospitalized due to their higher rate of comorbidities, use of immunosuppression medications, and increased risk of complications. As of April 2023, over 12,000 total transplants have been performed in our institution, of which, 538 (4.5%) have been lung transplants. Literature has demonstrated that hospitalist co-management services can reduce morbidity, 30-day readmission rates, and cost of care for various populations, such as orthopedic and neurosurgical patients. To build on these benefits of a hospitalist co-management model, a dedicated co-management service line for lung transplant recipients was created.
Purpose: Previously, hospitalized lung transplant recipients were cared for by the cardiothoracic surgery service for all hospitalizations. This model of care placed an undue burden on cardiothoracic surgeons, fellows, and medical transplant physicians given the complexity of care involved in the medical management of this population. As such, in 2017, the decision was made to create a co-management service line between the hospitalists and the lung transplant team.
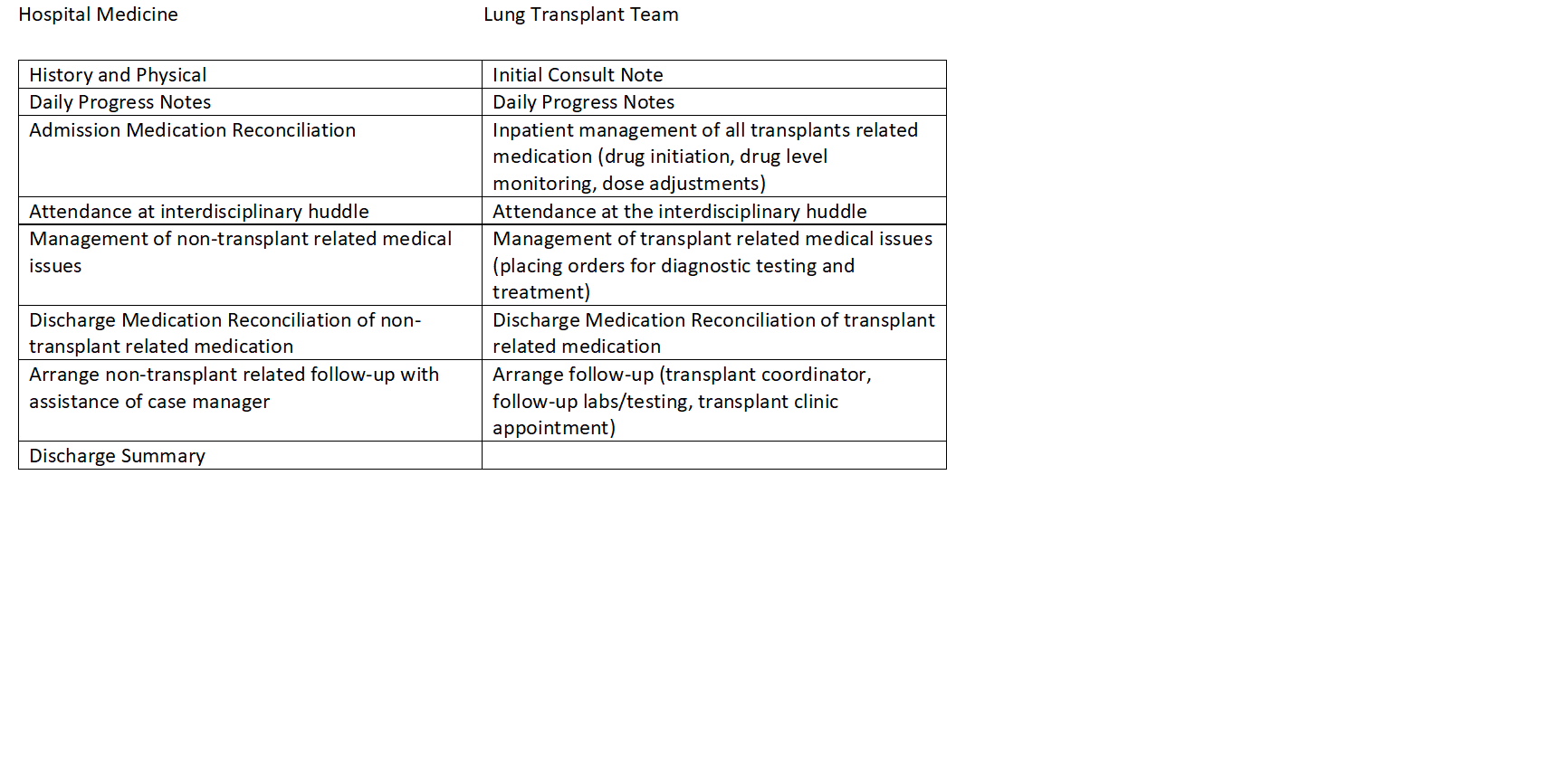
Description: Inclusion criteria included patients with a history of a lung transplant who were greater than 1 year from transplant. The patients who were excluded were those requiring intensive care level of support at the time of admission and/or requiring acute surgical management. Patients were admitted to a dedicated hospitalist service with collaborative management by a lung transplant provider where both teams rounded on each patient daily. Additionally, there is a multidisciplinary huddle every morning which includes the hospitalist, a provider from the transplant team, case manager, nursing, and physical therapist. Patients were cohorted to a single unit allowing for specialized nursing, pharmacist and case management for this niche population. Hospitalists were provided specialized lung transplant management education via lectures from transplant physicians at division Grand Rounds. In 2019, this program was expanded to include all lung transplant recipients that were admitted for a nonsurgical diagnosis and not requiring ICU level of care after the recipient’s index admission.Since July 2017 to date, there have been 749 lung transplant admissions to this service. Offloading the inpatient care management from surgeons allows for increased surgical productivity along with decreased provider burden and burnout. The creation of this co-management service also aided in the expansion of the lung transplant program. In 2020, our lung transplant program ranked in the top ten in the United States for volume and ranked first in our state for lung transplantation outcomes.
Conclusions: To our knowledge, this is the first discussion of a co-management of hospitalized lung transplant recipients. There has been prior robust data from other hospitalist-specialist co-management models, showing improved outcomes. We have created a framework for co-management between hospitalists and transplant medicine trained providers for this niche patient population and will use this groundwork to assess for improvements in hospital wide metrics while also considering further co-management services for other specialized patient cohorts.