Background: Multiple educational modalities have been utilized to teach high value care to trainees, including lectures, facilitated group discussion, and behavioral nudges and prompts (1–3). However, little has been done to compare different educational strategies delivered via the same modality. The goal of this study was to explore whether different educational prompts encouraging thoughtful lab ordering would lead to decreased lab utilization among internal medicine residents.
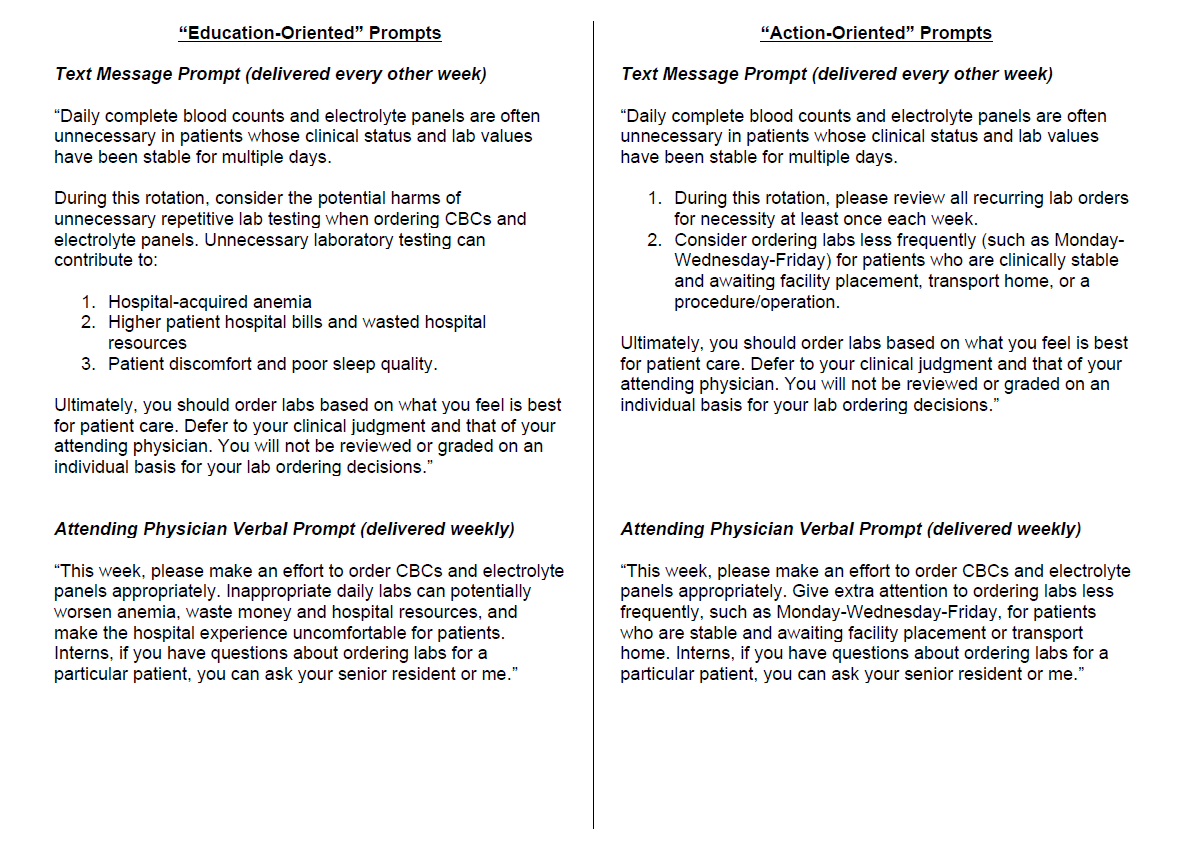
Methods: Two prompting protocols were developed to encourage thoughtful lab utilization. “Education-oriented” prompts emphasized harms of wasteful lab testing while “action-oriented” prompts suggested specific steps to mitigate daily lab orders, such as changing order frequency to Monday-Wednesday-Friday (see Figure 1). Both categories included weekly verbal prompts delivered by attending physicians and biweekly text messaging prompts such that residents would receive four verbal prompts and two text prompts during a four-week rotation. Prompts were drafted by authors VR and CJM, revised through iterative team review, and analyzed with language editing software to ensure similar readability. Pre-intervention data was collected from September to December 2022. Three internal medicine teaching services at an urban academic teaching hospital were then randomized to one of three intervention arms (education-oriented prompts, action-oriented prompts, and no prompts) for the 24-week intervention, which ran from January to June 2023. Hospital encounters were excluded if length of stay was less than three or more than 28 days or if any portion of the hospitalization was spent in intensive care. Primary outcome was average number of lab tests (complete blood counts and comprehensive metabolic, renal function, and basic metabolic panels) ordered per patient day per encounter.
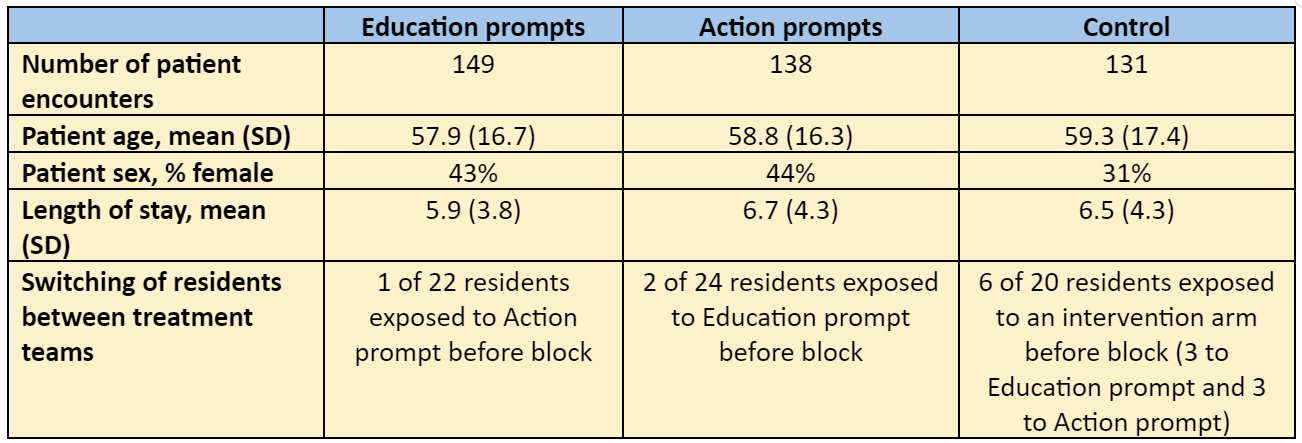
Results: In the pre-intervention and intervention periods, the teaching service receiving education-oriented prompts ordered 2.10 and 2.19 labs/day (p=0.21), the teaching service receiving action-oriented prompts ordered 2.11 and 1.98 labs/day (p=0.093), and the control service ordered 2.04 and 2.14 labs/d (p=0.19), respectively. Patient characteristics and resident switches between teams were similar between intervention arms in the pre-intervention and intervention periods (see Table 1).
Conclusions: In this preliminary analysis of a single-site educational intervention, no pre-post change in lab utilization was noted among medicine teaching services who received education- or action-oriented prompts encouraging appropriate lab utilization, although the action-oriented prompt team saw a modest decline in lab orders that approached statistical significance. This unadjusted analysis is limited by risk of confounders, including patient and physician heterogeneity. Next steps are to complete data cleaning and statistical analysis, including controlling for patient and physician characteristics.