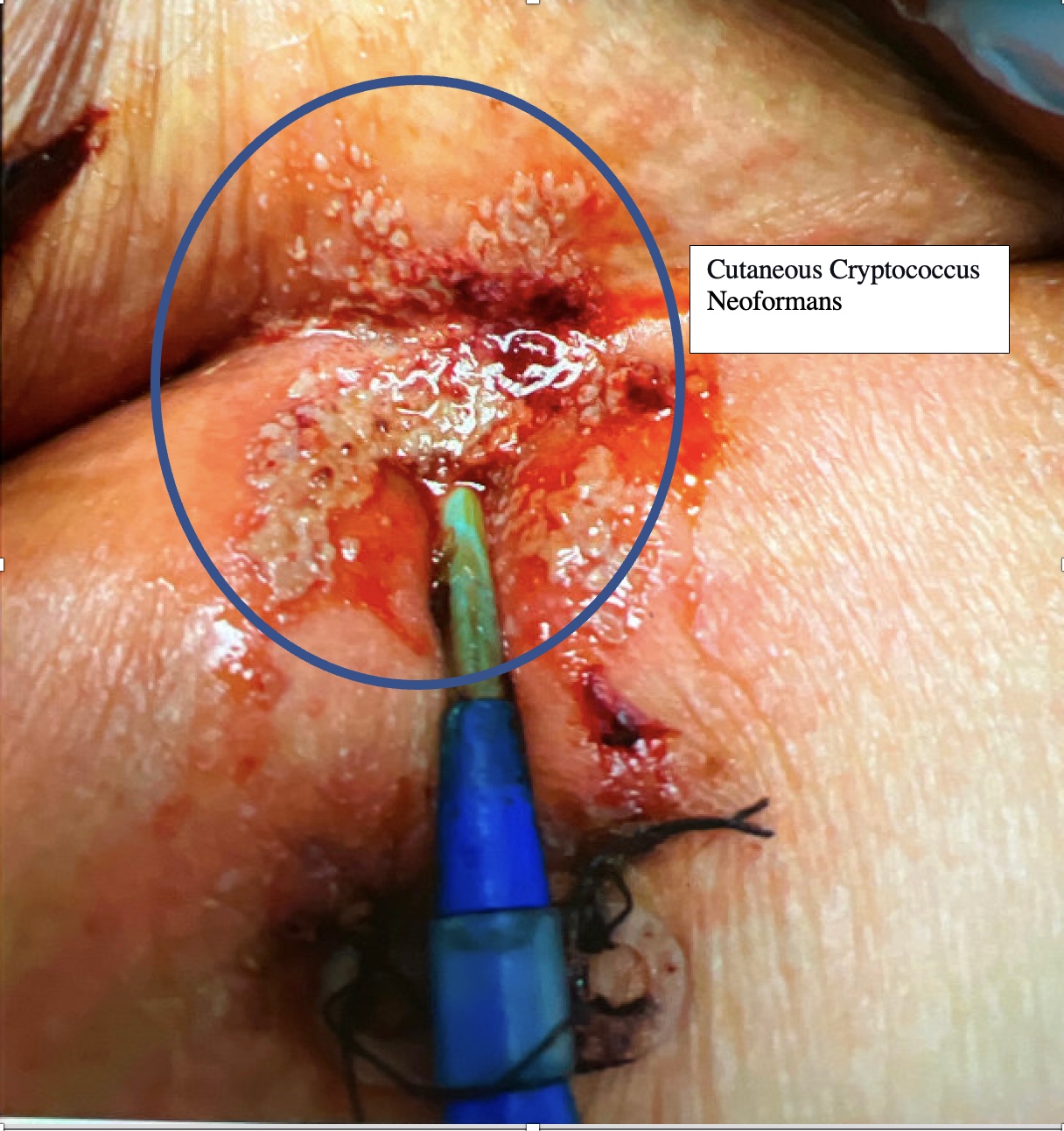
Case Presentation: A 58 year-old man with a past medical history of Chronic Obstructive Pulmonary Disease, poorly controlled Diabetes Mellitus (HbA1C 9.5%), and Hepatitis C with liver cirrhosis, presented with acute respiratory distress syndrome due to bibasilar community acquired pneumonia, eventually requiring extracorporeal membrane oxygenation. His hospital course was further complicated by empyema requiring placement of bilateral chest tubes, anuria requiring continuous renal replacement therapy (CRRT) through a femoral line, and multiple debridements for culture negative sacral decubitus abscesses. Due to very poor vascular access, replacement of his central venous access was not possible, and the same indwelling femoral central line was maintained for over a month for CRRT following which the patient developed a fever of 102⁰F. The patient was initially started on broad-spectrum antibiotics, although viral panels, blood cultures, and bronchoalveolar lavages including a fungal bronchial lavage, and sputum cultures were all negative. During this time, umbilicated papules consistent with cutaneous cryptococcus were seen around the femoral line, so fungal blood cultures were collected, and the patient was empirically started on fluconazole. On day 4, the fungal blood cultures grew Cryptococcus Neoformans; Flucytosine and Amphotericin B were initiated. HIV testing was subsequently done and the patient was negative with a CD4 count of 474 cells/mm^3. A lumbar puncture was performed and revealed an elevated opening pressure of 28mmHg with CSF analysis showing cryptococcal antigen titer (> 1: 2560). The patient unfortunately passed away prior to obtaining skin biopsies or completing his course of antifungals.
Discussion: There are two major pathological variants of the cryptococcus species: Cryptococcus neoformans and Cryptococcus Gatti. C. neoformans related infections are more common in those individuals who are immunocompromised, such as those with AIDS, end-stage liver disease, and chronic kidney disease. This fungus is endemic to America and found in soil. Spore inhalation primarily affects the lungs of immunocompromised patients and can disseminate to the central nervous system and the skin. However, primary cutaneous cryptococcus lesions are found in both immunocompetent and immunocompromised individuals, presenting as various skin manifestations, including umbilicated papules resembling Molluscum contagiosum. It is suspected that in our patient, primary Cutaneous Cryptococcus lesions led to disseminated Cryptococcosis by forming a biofilm around the catheter in the setting of the patient’s immunocompromised state. The solitary cutaneous manifestations of Cryptococcus seen only localized around the femoral line coupled with the prior negative fungal bronchoalveolar lavages support this conclusion.
Conclusions: Patients who must have the same central line in place for longer than 14 days are at higher risk for central line-associated bloodstream infections. For this reason, clinicians should thoroughly inspect the skin near the catheter insertion site. If suspicious skin lesions are seen, and patients develop sepsis with negative bacterial workups, clinicians should have a high suspicion for fungal infections, including Cryptococcus. If cutaneous manifestations are present, fungal blood cultures, CSF studies, and skin biopsies should be considered to rule out disseminated Cryptococcosis, and prompt life-saving antifungals can be administered.