Background: Hospital systems are increasingly focusing on health equity, including identifying and addressing social drivers of health and healthcare disparities. Conventional quality improvement (QI) approaches have been used to address disparities with varying success. In our health system, using QI to increase use of interpreters has been the primary intervention for improving outcomes in patients with Limited English Proficiency (LEP). We sought to develop a more comprehensive approach to improving care by partnering with experts in systems design.
Purpose: To create a collaborative, transdisciplinary model informed by systems design approaches to guide our efforts to improve hospital-based care for patients with LEP.
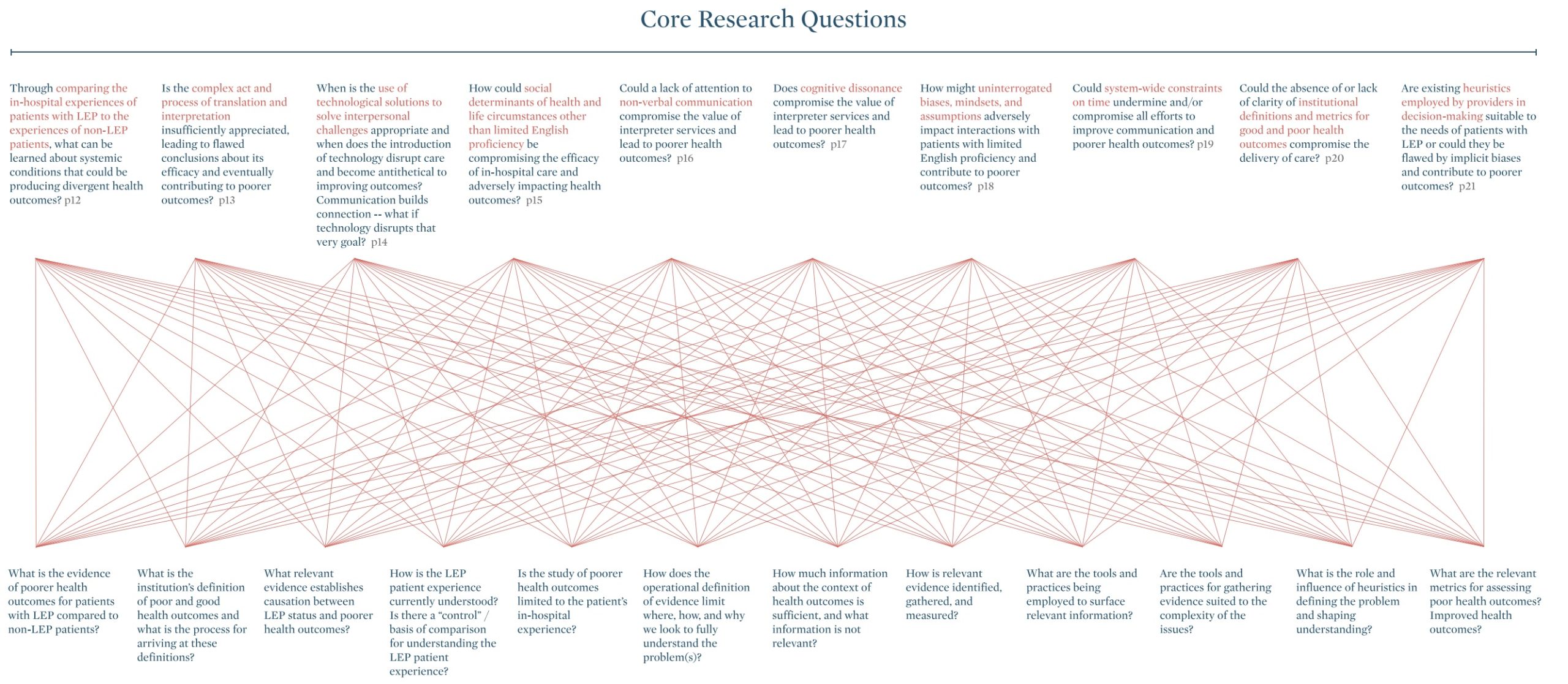
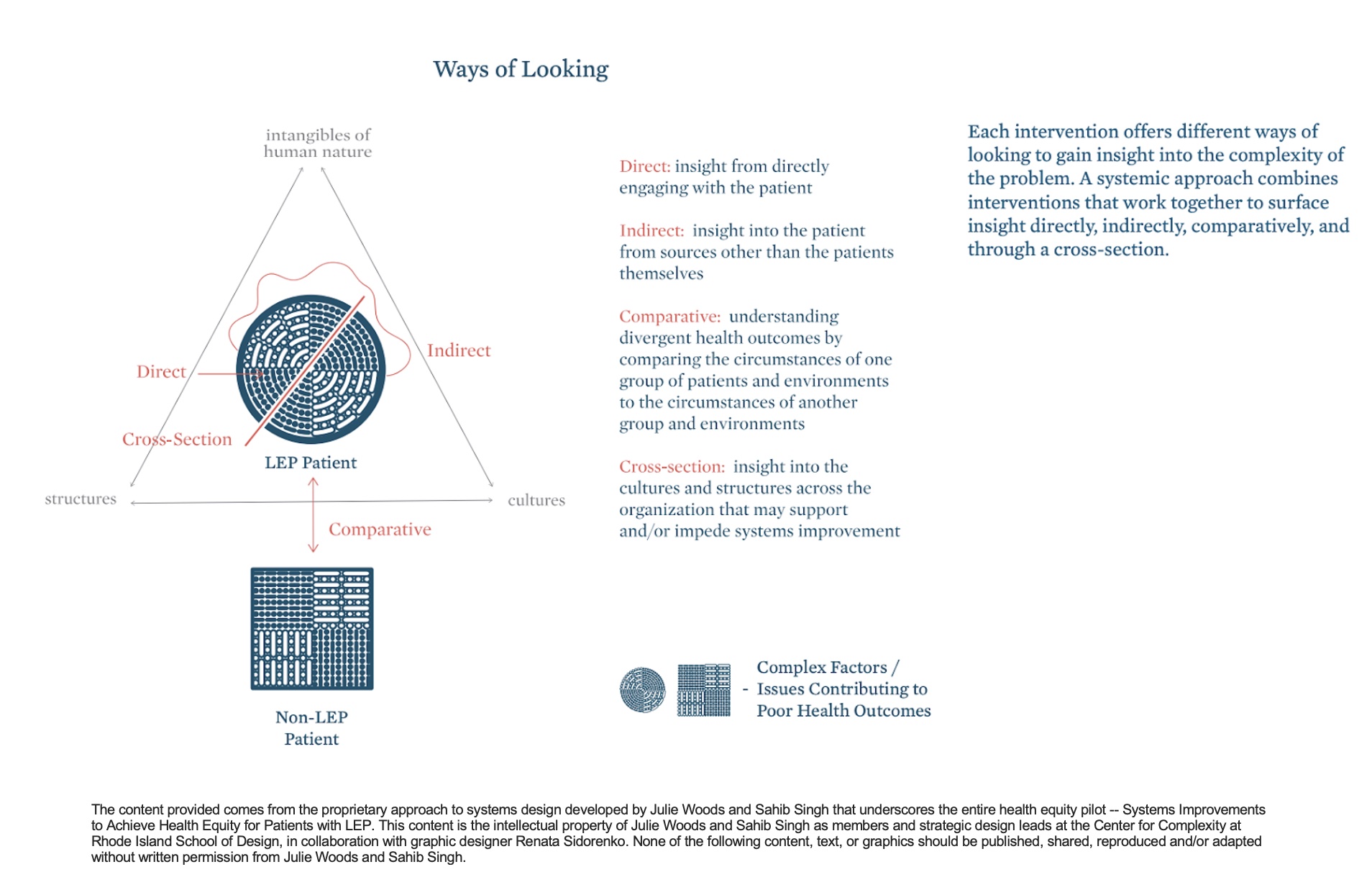
Description: After five years of using traditional QI methods to improve care for patients with LEP with moderate success, our division, which is based in an urban academic health system, forged a partnership with systems designers from a School of Design, embarking on a comprehensive reevaluation of our health equity approach for individuals with LEP. Over the course of two years, our partners used systems design methodology to help elucidate a wide range of contributors to health disparities for patients with LEP while simultaneously identifying areas for potential improvement efforts. As a voluntary partnership with multiple participants, the traditional “studio approach”, a component of systems design, was adapted to fit the needs of our participants. Monthly meetings for the first year, the Pre-Studio phase, allowed time to understand what was known about disparities in care for patients with LEP. This process broadened our research questions (Image 1) by allowing us to step back and question the parameters of the problem, identify relevant lines of inquiry, and develop an understanding of systems issues. The Studio Phase over the following 6 months applied creative practices to explore the assumptions and biases in the group’s logics and proposed solutions. We successfully obtained a grant of $100,000 to launch a 30-week pilot program. The program consisted of developing 11 specific paths of inquiry, “prototypes”, aimed at comprehending the systemic factors contributing to nonequivalent care for patients with LEP when compared to their English-speaking counterparts. Each prototype was crafted through iterative collaboration to study the intricate interactions between patients, healthcare providers, health systems, and broader societal and cultural factors (Image 2). Direct patient insight was prioritized with the majority of prototypes involving patient interviews. Transdisciplinary medical professionals from the Division of Hospital Medicine, Interpreter Services, and Case Management serve as on-site leads for each prototype.
Conclusions: This innovation challenges the conventional belief that language and interpretation alone drive health disparities for patients with Limited English Proficiency (LEP). The dual-pronged pilot initiative seeks to uncover the underlying structures influencing healthcare outcomes for this population before actively testing hypotheses through targeted interventions. Systems design-informed improvement work is a novel approach to advancing health equity by applying creative and patient centered practice to identify, understand, and address the factors perpetuating poor outcomes.