Background: As more hospitalists have gained basic point-of-care ultrasound (POCUS) skills, the desire for training in more advanced POCUS applications has increased as well as the need for developing faculty with an advanced POCUS skillset, that can support expansion of training and clinical integration into practice. Current certificate and credentialing pathways help build basic POCUS skills through workshops, modules, and portfolios, but a significant gap remains between the final skillset acquired and the skills needed for hospitalist faculty to expand clinical utility and educate others in POCUS. To address this gap, we developed a novel curriculum with three main objectives: (1) solidify understanding of tomographic planes and image optimization, (2) emphasize POCUS clinical integration through evidence-based approaches, and (3) introduce new, clinically useful advanced techniques. We hypothesized that course participants, who possessed basic POCUS skills, could achieve significant improvement in image acquisition and subsequent application of advanced techniques.
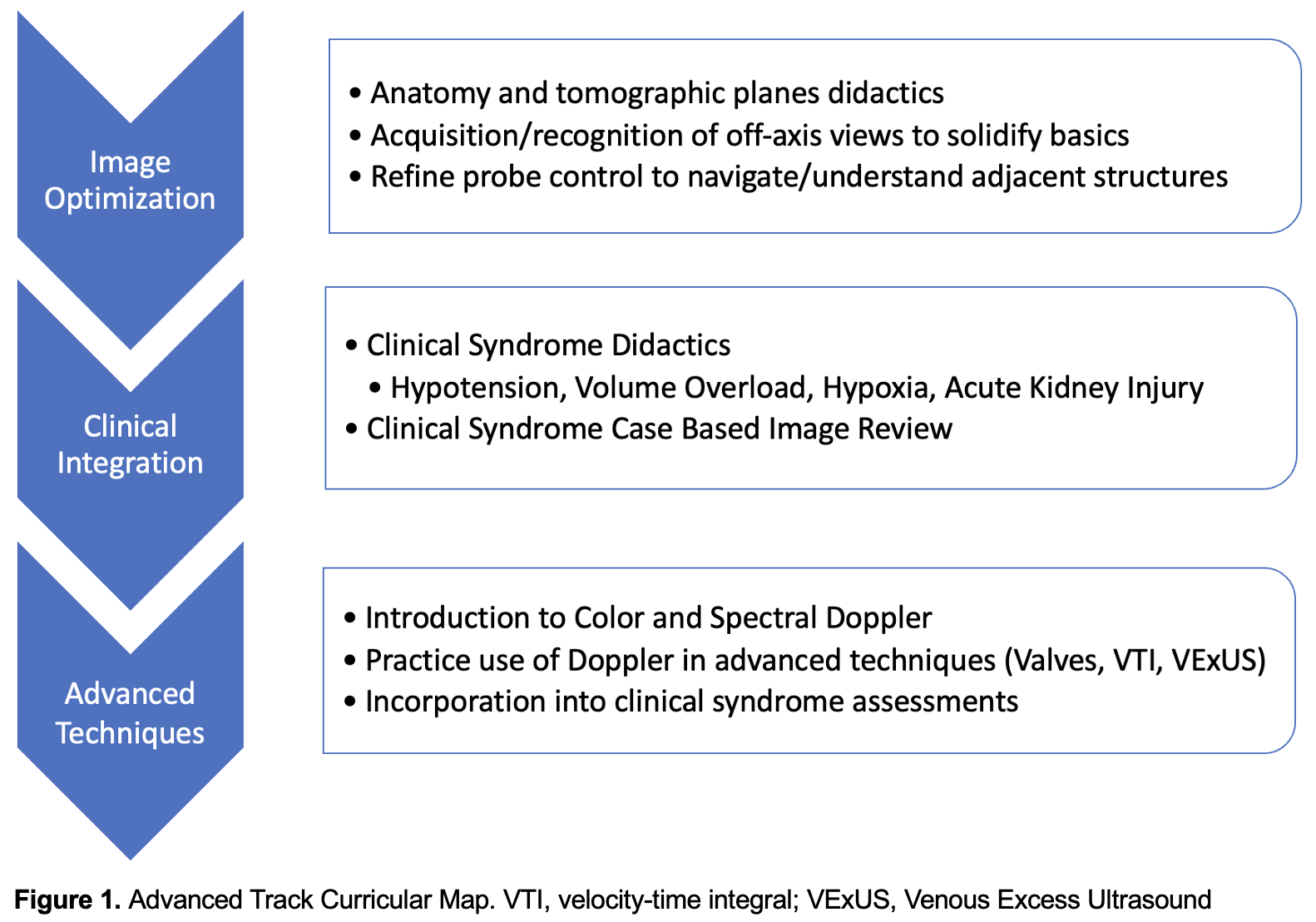
Methods: During an established two-day POCUS continuing medical education workshop, a separate advanced track was offered in-parallel with the traditional basic track. In the 6 months prior to the course, faculty with POCUS curriculum development experience formed an advanced track curriculum to meet the above outlined objectives (Figure 1). Advanced track course participants (n=18) were self-selected without inclusion criteria. All were asked to complete a pre-course written test, to ensure they had basic POCUS knowledge, and none needed to be excluded based on these results. To assess the effectiveness of the advanced track curriculum, we used standardized pre- and post-course tests and surveys to anonymously assess learner perspectives, knowledge, and image acquisition skills.
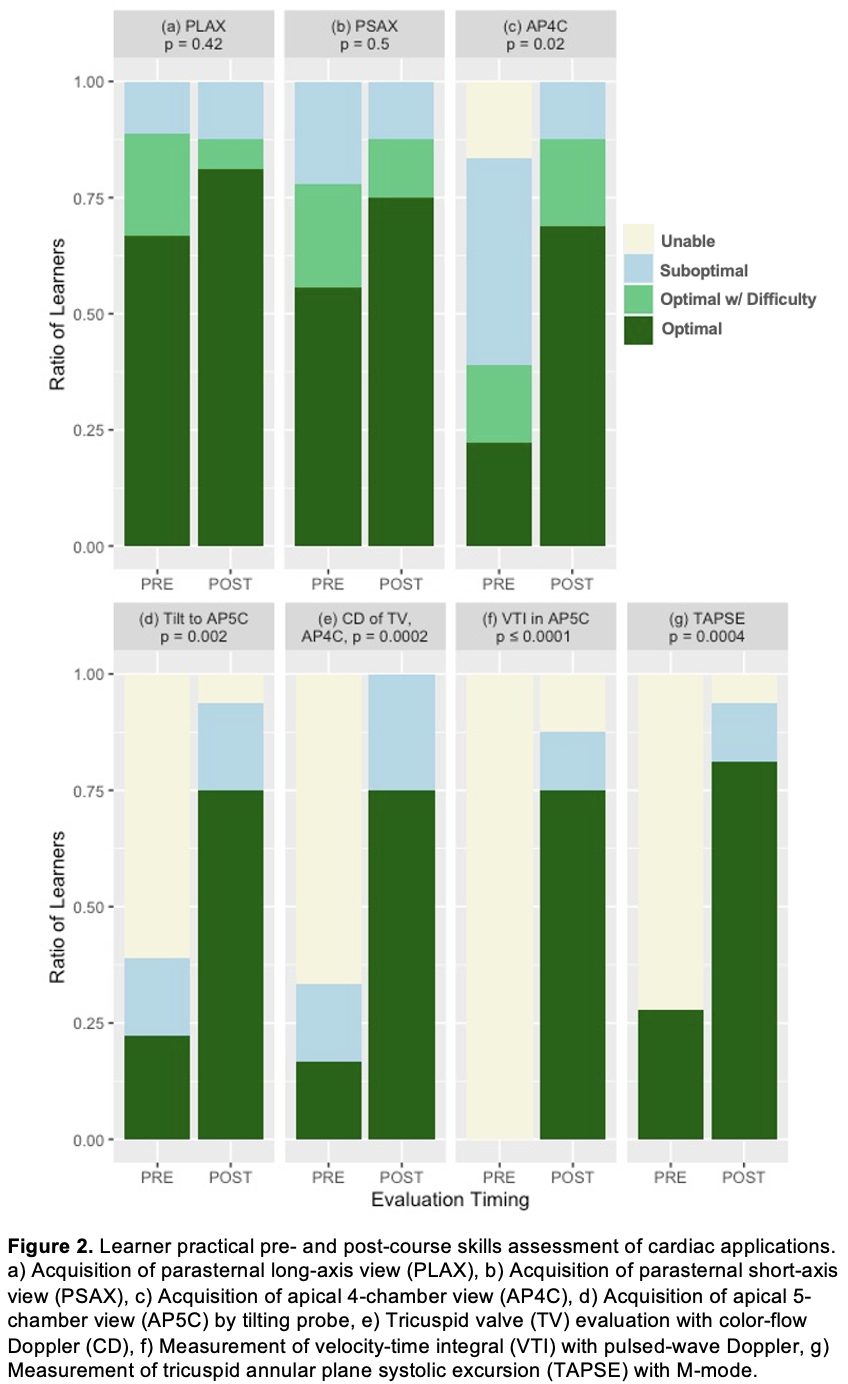
Results: Most participants reported ≥25 hours of prior POCUS training (78%), were using POCUS at least weekly (67%) and were teaching POCUS to others (83%). Of the 3 basic cardiac views (parasternal long- and short-axis and apical 4-chamber views), participants demonstrated the most improvement in acquiring optimal apical 4-chamber views (22% vs 69%, p=0.02). Course participants also improved their ability to use color-flow Doppler to evaluate the mitral and tricuspid valves with most demonstrating optimal use (0% vs 63%, p< 0.001 and 17% vs 75%, p< 0.001, respectively). Acquisition of advanced cardiac views, including the right ventricular inflow (0% vs 69%, p< 0.001), apical 5-chamber (22% vs 75%, p=0.002), and apical 3-chamber (0% vs 50%, p< 0.001) view, also improved. Finally, significant improvement was seen in assessment of tricuspid annular plane systolic excursion (TAPSE) (28% vs 81%, p< 0.001) and left ventricular outflow tract velocity time integral (0% vs 75%, p< 0.001) post-course (Figure 2).
Conclusions: By adapting the structure of a basic POCUS workshop to deliver a novel advanced POCUS curriculum, we demonstrated improvements in POCUS users’ skillsets that better match the advanced clinical and educational needs of many hospitalists. Our data suggests that this approach was effective at improving observed visuospatial understanding and image acquisition skills in basic and advanced techniques.