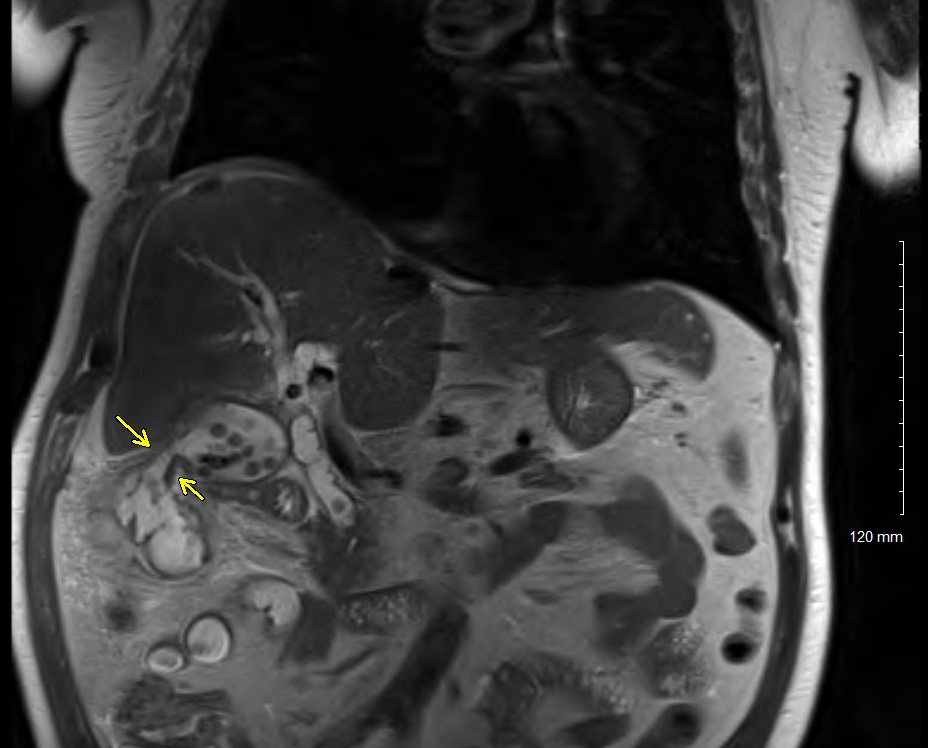
Case Presentation: A 59-year-old incarcerated male presented to the hospital with abdominal pain, fever, and vomiting. Initial diagnostic workup showed a total leukocyte count of 14.2 x 103 /uL. The alkaline phosphate and total bilirubin were normal at 73 IU/L and 1.2 mg/dL, respectively. The Computerized tomography (CT) with contrast of the abdomen and pelvis revealed a distended gallbladder with thickened walls and a complex fluid collection of 11.5 x 3.8 cm near the subcapsular region of the dome of the right liver lobe. The patient was started on broad-spectrum antibiotics and discharged with clinical improvement. The patient was admitted again with ongoing fever and abdominal pain. This time, an Ultrasound of the abdomen showed persistence of gall bladder distention and right liver abscess. Hepatobiliary Scintigraphy (HIDA scan) showed no visualization of the gall bladder, confirming acute cholecystitis. Magnetic resonance cholangiopancreatography (MRCP) showed gallstones in the common bile duct (CBD) and a fistula between the gall bladder wall and hepatic flexure of the colon with associated colon wall inflammation [image]. Our patient underwent multifaceted interventions for acute cholecystitis, choledocholithiasis, liver abscess, colon thickening, and Cholecystocolonic fistula. Endoscopic Cholangiopancreatography (ERCP) was performed for CBD stone extraction. During surgical exploration, hepatic flexure of the colon was inseparable from the gall bladder and the liver edge, requiring a right hemicolectomy with ileocolic anastomosis, drainage of hepatic abscess, and cholecystectomy with fistula repair. The histopathological evaluation of the surgical specimen revealed severe hemorrhagic xanthogranulomatous gall bladder inflammation. Postoperative recovery was uneventful, and the patient was discharged on oral antibiotics for two weeks.
Discussion: Cholecystocolonic fistulas (CCF) represent a rare but severe late complication of untreated gallstone disease. It is discovered in approximately 0.1% of cholecystectomies. It is often associated with several other complications, such as acute cholangitis, biliary peritonitis, and biliary cirrhosis, with an overall mortality rate of 10% to 15% [1]. Due to the elusive presentation and a wide range of symptoms, CCF remains a diagnostic challenge. The pathognomonic triad of pneumobilia, chronic diarrhea, and vitamin K malabsorption was not observed in our patient [2]. Our case underscores the importance of maintaining a high index of suspicion for Cholecystocolonic fistula in patients with recurrent abdominal symptoms with complex biliary disease and abnormal hepatic flexure thickening of the colon. Timely diagnosis and surgical intervention could potentially halt clinical deterioration and further complications.
Conclusions: The clinical odyssey of this patient accentuates the necessity for a meticulous and multidisciplinary approach to managing complex hepatobiliary conditions, especially in our patients with readmission and escalating symptoms.