Background: The volume of opioid prescriptions in the US has increased dramatically over the last two decades, and strong evidence suggests that this has perpetuated opioid misuse, addiction, overdose, and drug-related deaths. We aimed to learn if there are differences in opioid prescribing among generalist physicians, NPs, and PAs to Medicare beneficiaries.
Methods: We performed a cross-sectional analysis of prescription claims from 2013 to 2016 using data from CMS for Medicare Part D beneficiaries. All generalist physicians, NPs, and PAs who provided more than ten total prescription claims between 2013 and 2016 were included. These prescribers were subsetted as practicing in a primary care, urgent care, or hospital-based setting. The main outcomes were total opioid claims and opioid claims as a proportion of all claims to patients treated by these prescribers in each practice settings. Binomial regression was used to generate marginal estimates to allow comparison of the volume of claims by these prescribers with adjustment for practice setting, gender, years of practice, median income of the zip code, state fixed effects, and relevant interaction terms.
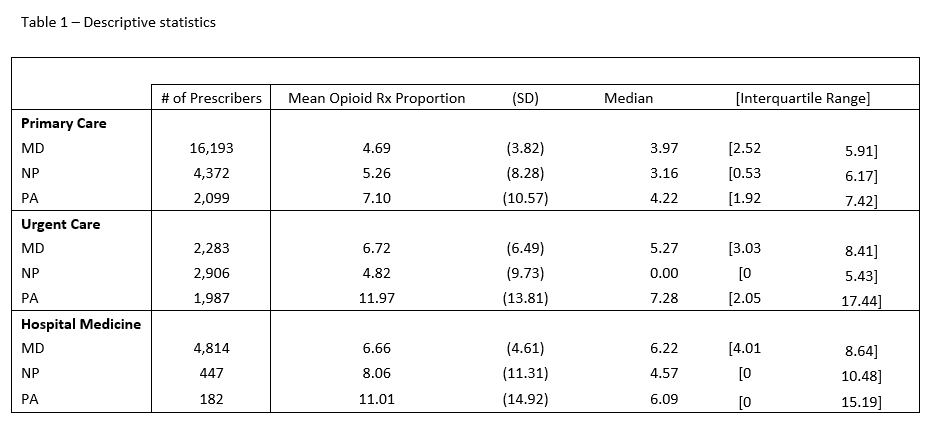
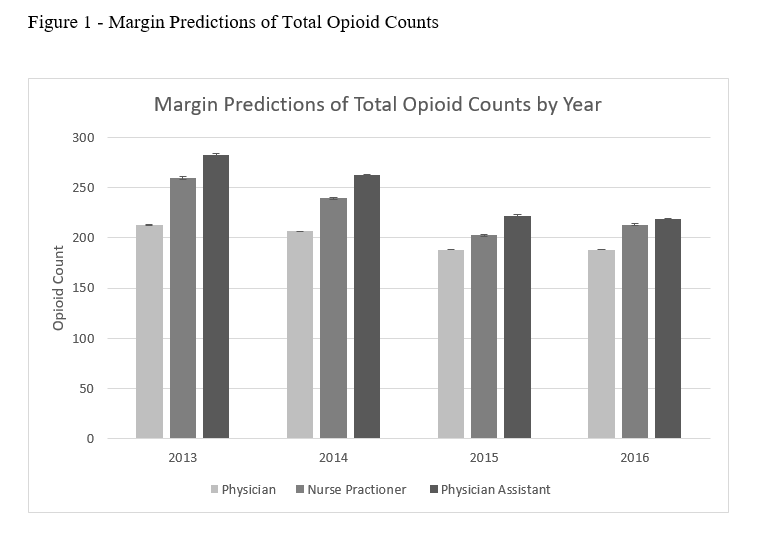
Results: There were 36,999 generalist clinicians (physicians, NPs, and PAs) with at least one year of drug claims data. The distributions of total opioid claims for all thee practitioner types were extremely right-skewed but clustered around zero. The mean opioid prescription proportions (as a proportion of all prescription claims) for physicians in primary care, urgent care, and hospital medicine were 4.69, 6.72, and 6.66 relative to 7.10, 11.97, and 11.01 for PAs (Table 1). The adjusted total opioid claims across these four years for physicians was 660 (95% CI: 660-661), for NPs was 755 (95% CI: 753-757), and for PAs was 812 (95% CI: 811-814). In the analysis by year, there was a decreasing trend in prescribing for each generalist type (Figure 1).
Conclusions: We found that generalist NPs and PAs may be prescribing a disproportionately high quantity of opioids to Medicare patients relative to generalist physicians. One potential explanation is that pharmaceutical companies are specifically targeting generalist NPs and PAs (this is support by claims from several state attorney generals). Understanding this trend could help determine points for interventions to reduce opioid prescribing.