Background: Unnecessary laboratory orders are a well-known contributor to healthcare cost. Our residents identified “fear of attending” as a barrier to more mindful lab ordering. This project focused on educating attending physicians on high-value care and promoting resident-attending discussions.
Purpose: Data was collected via anonymous pre and post-intervention survey (designed by the study team). Participants included resident and attending physicians on the inpatient Medicine service. Multiple interventions targeting attending physicians occurred over a 16-week period including presentations at the monthly hospitalist meeting (included resident lab-ordering data and resident perceptions of attendings). Electronic requests asked attendings to voluntarily submit a message of support for the project; these were then shared with residents. An attending project champion was identified and emailed attendings on service with reminders to discuss lab ordering with their teams. Surveys assessed sustainability at 6 months and 1 year.
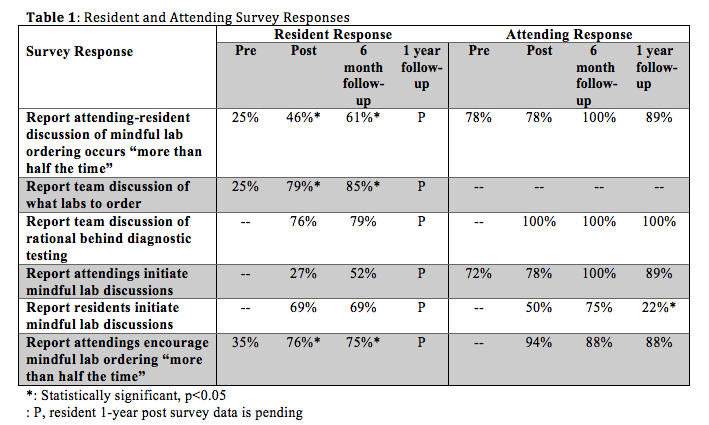
Description: Initially, 70% of residents reported worrying about repercussions from attendings if daily labs were not ordered; at 6 months, only 24% reported this (p<0.05). Residents receiving “pushback” from attendings for not ordering daily labs increased from 25% to 54% (statistically significant, p<0.05) which sustained at 6 months. At 6 months, 71% of interns and 51% of senior residents reported receiving “pushback” from attendings. After the interventions for 16 weeks, 62% of attending physicians reported that residents are appropriately mindful of laboratory orders (sustained at 6 and 12 months). Survey results listed in Table 1.
Conclusions: Our data shows a discrepancy in the perception of mindful ordering discussions between resident and attending physicians. Attendings have a higher perception of attending-initiated discussions and a lower perception of resident-initiated discussion. Interestingly, between 6 and 12-month follow-up, attendings report a decrease in resident-initiated discussions. We hypothesize that this is secondary to a new academic year or may indicate a new barrier. The increased resident-reported discussion of lab ordering has sustained through 6-months. This is further supported by the attendings perceiving the residents as being appropriately mindful of laboratory orders. However, residents have reported receiving more pushback from attendings. This may suggest that attendings are more resistant to mindful lab ordering than they perceive or may reflect increased effort by residents to change lab ordering practices. Despite pushback, fewer residents fear attendings’ repercussions. Our data suggests a cultural shift at both the attending and residents levels but additional work remains. Medicine’s hierarchical structure results in attending physicians’ strong influence on resident ordering practices. It is crucial for attending physicians to promote high-value, cost-conscious care through team discussion and a positive learning environment for a sustainable high-value care culture.