Background:
Although it is widely recognized that type II diabetes (DM) is associated with diastolic dysfunction (DD), and despite increasing evidence that diabetic lung disease is more prevalent than generally recognized, it is unknown which one of these factors contributes more to dyspnea in diabetic patients.
Methods:
We reviewed medical records for all adult patients presenting with dyspnea and undergoing pulmonary function testing (PFT) and echocardiograms in our institution between January 2004 and December 2005. In a cross‐sectional analysis we used multivariable logistic regression to examine the association between DM and different ventilatory patterns. We defined restrictive pattern (RE) as FVC < 80% and FEV1/ FVC ≥ 70% and obstructive pattern (OB) as FEV1 < 80% and FEV1/ FVC < 70% of predicted values. Further, we selected all patients with DM who had undergone both PFT and echocardiogram, and we assessed the prevalence of RE and OB patterns and the presence of diastolic and systolic dysfunction.
Results:
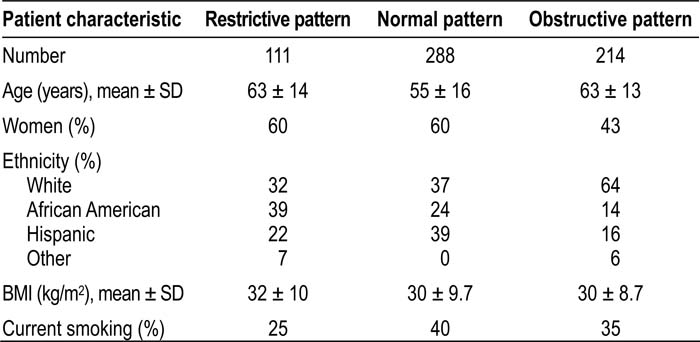
Among 613 patients with dyspnea undergoing PFT, 288 (47%) had normal (NL), 214 (35%) had OB, and 111 patients (18%) had RE ventilatory pattern (Table 1). There were more diabetics in the RE than in the NL and OB groups (43% vs. 17% and 19%). After adjustment for age, BMI, sex, ethnicity and smoking, RE pattern was independently associated with DM (OR 3.5, 95% CI 1.85‐6.62), whereas OB pattern was not (OR 0.77, 95% CI 0.35‐1.66). Among 152 diabetics presenting with dyspnea in our study, 60 (39%) had RE only, 20 (13%) had DD only, 30 (20%) had both RE and DD, whereas the rest had either an NL (20%) or OB (8%) ventilatory pattern.
Conclusions:
Restrictive ventilatory pattern is independently associated with diabetes. Dyspnea in diabetic patients is a result of a restrictive ventilatory pattern rather than diastolic dysfunction. In the new era of inhaled insulin, a better understanding of lung dysfunction in diabetics is needed in order to differentiate between lung toxicity due to chronic hypergly‐cemia and the potential side effects of inhaled insulin.
Author Disclosure:
O. Klein, none; F. Flores, none; M. Samee, none; J. Brenkley, none; D. Tate, none.