Background: Over the past fifty years, remote cardiac monitoring (“telemetry”) has become routine for many patients admitted to the hospital. Telemetry has many clinical benefits and is recommended by the American Heart Association for a limited set of indications, but is often inappropriately used. Overutilization of telemetry can lead to unnecessary tests and procedures, may contribute to increased cost of care and alarm fatigue, and could lead to patient harm. Previous studies have looked at reducing unnecessary use of telemetry through a variety of interventions. However, the effect of removing default settings in admission order sets on telemetry ordering by physicians is not known.Soon after implementation of a vendor electronic health record at our institution, a customized admission order set was developed for internal medicine residents in which telemetry was preselected. Due to high rates of inappropriate telemetry usage, this default selection was deactivated in Fall 2017. We were interested in examining the effects of removing the preselected telemetry order from the admission order set in this natural experiment. Our hypothesis was that telemetry ordering would decrease when the order was no longer preselected.
Methods: This controlled, pre-post study was conducted at a large academic medical center. We analyzed orders for all patients admitted to a general medicine service covered by residents 60 days before and after the default setting was changed. Using a chi-squared statistic to compare the pre- and post-month along with an interrupted time series analysis , we compared the number of times telemetry was ordered from the Residency Order Set (ROS) before and after deactivation. To control for temporal trends, we similarly analyzed two different order sets that did not have their telemetry preselections changed (one order set had the order preselected and the other did not) during this time period.
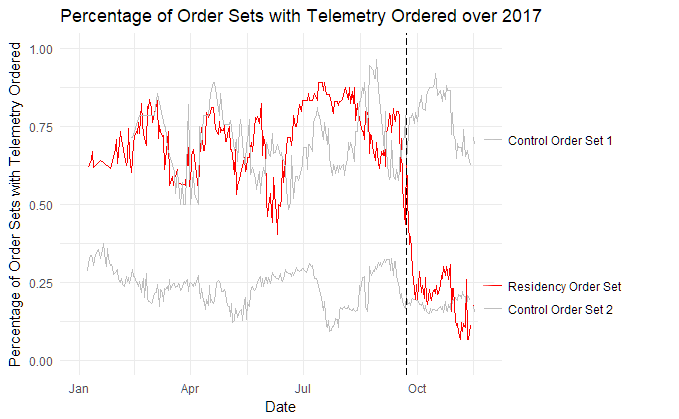
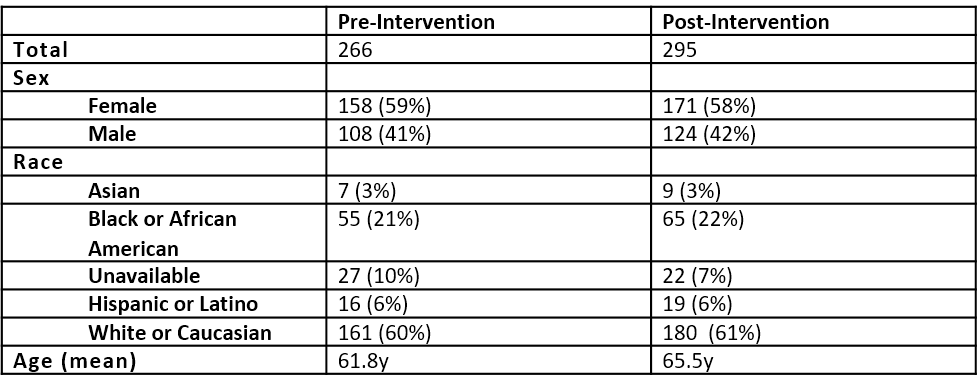
Results: Two hundred and sixty-six patients were admitted using the ROS in the 60 days before deactivation, and 295 were admitted post (Table 1). Pre-intervention, 201 (76%) patients were ordered for telemetry on admission, compared to 67 (23%) post-intervention (p < 0.001). There was no clinically significant change in telemetry ordering from control order sets. A 14-day smoothed time series analysis is shown below (Figure 1). The interrupted time series analysis (Figure 1) was statistically significant (p < 0.001).
Conclusions: Removing telemetry as a preselected order in ROS led to a significant and dramatic decrease in telemetry ordering by residents. Our study underscores the potential consequences of including orders as defaults in order sets as well as impact on appropriate utilization of resources by trainees. Our data support the use of carefully selected order set defaults as a powerful tool to encourage appropriate ordering practices as part of hospital-based Choosing Wisely program.