Case Presentation:
A 62‐year‐old woman with diabetes presented with 4 days of crampy, epigastric pain exacerbated by urination and radiating to the right and left upper quadrants. She endorsed nausea and emesis but denied fever or association with food. A physical exam on presentation revealed that she was afebrile, tachycardic, and had a soft, obese abdomen with bilateral upper quadrant tenderness to deep palpation. Labs showed leukocytosis with bandemia, acute renal failure, and UTI. A CT scan showed an enlarged, nonhydro‐nephrotic right kidney with perinephric stranding and gas in the cortex and perinephric spaces. She was admitted to the ICU for management of emphysematous pyelonephritis (EPN). She initially developed DKA and septic shock requiring pressor support. Blood and urine cultures grew Escherichia coli. Nephrectomy was considered, but she instead received broad‐spectrum antibiotics and underwent percutaneous nephrostomy tube drainage (PCD) for kidney preservation. Serial CT scans showed substantial improvement, and she was later discharged home.
Discussion:
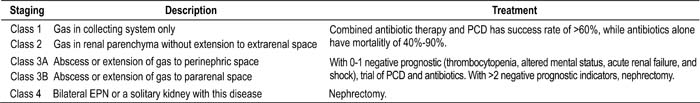
EPN is a rare, life‐threatening infection of the kidneys characterized by gas in the renal parenchyma, collecting system, or perinephric tissue. Occurring almost exclusively in poorly controlled diabetics, it affects women 6 times more frequently than men and occurs most often in the sixth to eighth decades of life. Escherichia coli and Klebsiella pneumoniae are the primary causative organisms. Tissue hyperglycemia causes the bacteria to thrive and produce gas through mixed‐acid fermentation of glucose. This coupled with impaired tissue perfusion and weakened immune response often presents in poorly controlled diabetics and provides a fertile environment for EPN to develop. The common presenting symptoms — fever, flank pain, and pyuria — are nonspecific. Clinical findings with significant negative prognostic value are thrombocytopenia, altered mental status, acute renal failure, and shock. EPN is diagnosed and classified based on CT findings. Treatment is based on disease class, as listed in Table 1.
Conclusions:
EPN should be suspected in diabetics with urosepsis and significant acute renal failure. Though rare, the projected growth of the diabetic population warrants increased attention to this potentially fatal disease. A successful outcome is possible through combined medical and surgical treatment.
Author Disclosure:
T. Deans, MD, none; S. Higgins, MD, none.