Background: Hospitals globally have been facing unprecedented challenges with patient throughput and capacity, especially in the aftermath of the COVID-19 pandemic. Efficient discharge processes are integral to improving bed availability and mitigating the negative outcomes associated with patient boarding in emergency departments
Purpose: This study evaluates the efficacy of an early morning huddle approach in improving early hospital discharges and decongesting hospital systems
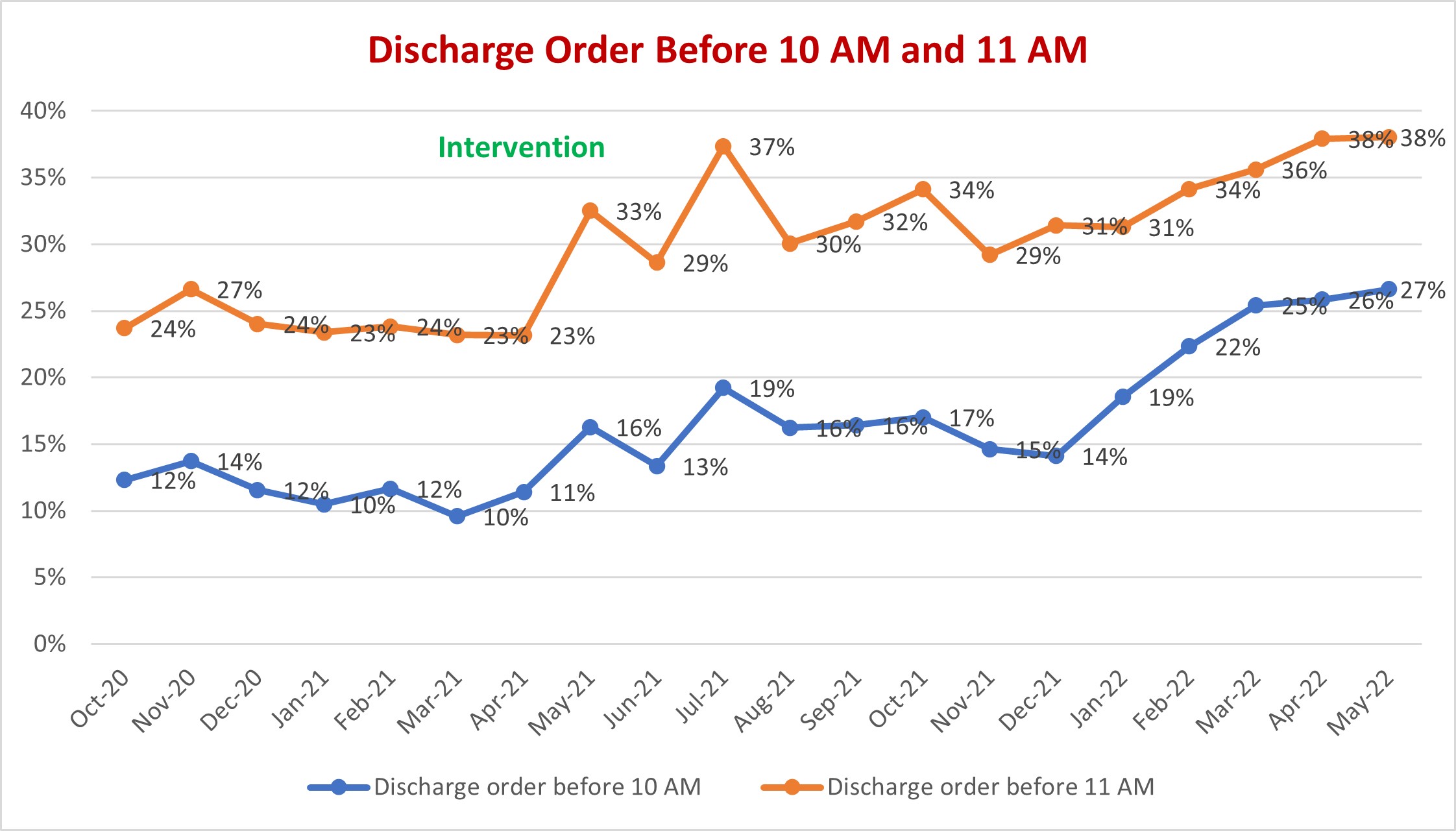
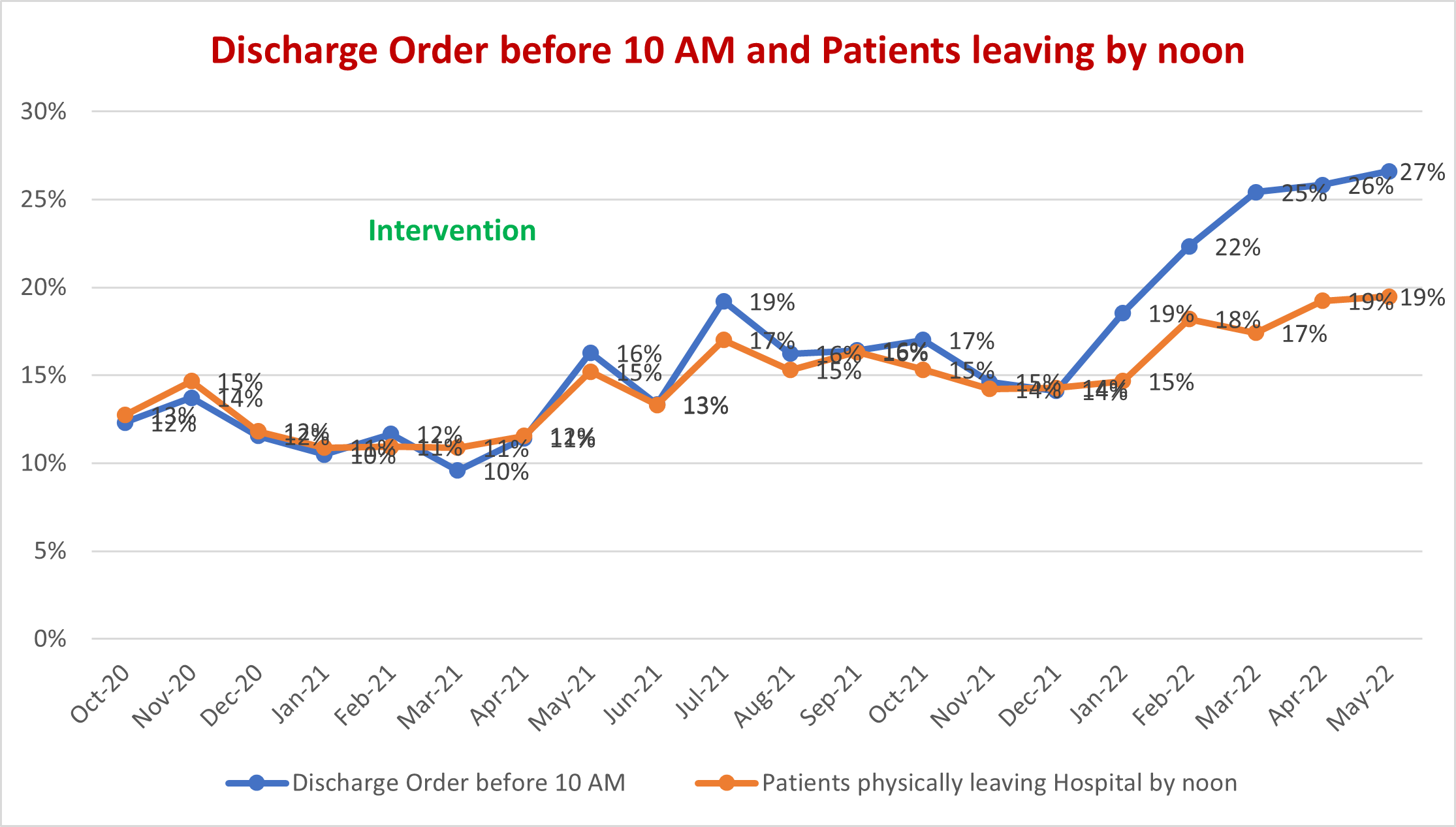
Description: This study employed a quasi-experimental design to evaluate the impact of implementing a structured early morning huddle on early discharges at Baystate Medical Center. Baystate Medical Center is a tertiary care center with approximately 720 beds, of which around 500 are covered by the Hospital Medicine Division. The intervention involved the implementation of a structured early morning huddle at 7:15 AM daily lasted for 15 minutes and was conducted virtually via Zoom to ensure minimal disruption to clinical duties. Hospitalists, the medical director, and a hospitalist resource nurse were the primary participants in these huddles. The meeting followed a predetermined script that facilitated efficient communication. The script included:1. Identifying potential discharges and issuing orders first thing in the morning.2. Identifying barriers such as diagnostic tests, imaging, and consultations that need completion before a patient can be discharged.3. Discussion on resource allocation, consult delays, and placement issues.The first five minutes of the huddle were led by the medical director, who provided an overview of issues for the day, such as the number of ED boarders, priorities, and recognition for hospitalists with the highest number of discharges the previous day. The subsequent ten minutes involved hospitalists reporting on early discharges and discussing potential barriers.Data Collection and Management:A hospitalist resource nurse created an Excel spreadsheet summarizing the information shared during the huddle. This spreadsheet contained data on potential discharges, barriers identified, and actions needed to expedite discharge. This information was then disseminated to nursing units, managers, and case managers for action. Through effective collaboration and communication, the barriers were addressed to expedite discharges.Prior to the implementation of the structured early morning huddle, the baseline data indicated that an average of 12% of discharge orders was placed before 10 AM. At one-year post-implementation, this percentage had increased to 25%, represented a 100% increase. The baseline data also indicated that about 12% of patients physically left the hospital before noon. One year after the implementation this percentage increased to 20%, represented a 75% increase. The paired t-test revealed that these increases were statistically significant (p < 0.05).
Conclusions: This study demonstrated that implementing a structured early morning huddle at a tertiary care center significantly increased the number of early hospital discharges. The huddle’s structured format, efficient communication, and a systematic approach to addressing discharge barriers contributed to the success of this intervention. Early hospital discharges have potential benefits, including increased bed availability, reduced patient boarding in emergency departments, and possibly improved patient outcomes by minimizing hospital-associated complications.