Case Presentation: A 36-year-old G9P9 Jehovah’s Witness female with no significant past medical history, presented to the emergency department with a 2-week history of postural headaches and double vision. Neurological examination was normal except for left abducens nerve palsy. CTA of the head was unremarkable, but an MRI of the head revealed diffuse smooth dural thickening with enhancement suggestive of intracranial hypotension. The patient reported a history of nine live births, with seven involving epidurals. A CSF leak was suspected as the cause of the intracranial hypotension. MRI of the whole spine showed diffuse smooth dural thickening with enhancement and extradural collections, however, no single point of leakage was identified. Based on her history and imaging, abducens nerve palsy was believed to be secondary to intracranial hypotension leading to brain displacement and traction on the left abducens nerve.Conservative treatment modalities including Caffeine and salt tablets did not result in significant clinical improvement. The treatment team felt an epidural blood patch was the next treatment option but we had to make sure it did not go against the patient’s religious beliefs. The patient consulted with the Elders of her Jehovah’s Witness community, and they felt that an autologous epidural blood patch procedure was in alignment with her beliefs as a Jehovah’s Witness. She reported significant improvement in her headache and mild improvement in her double vision after two blood patches were applied. She was discharged home thereafter.
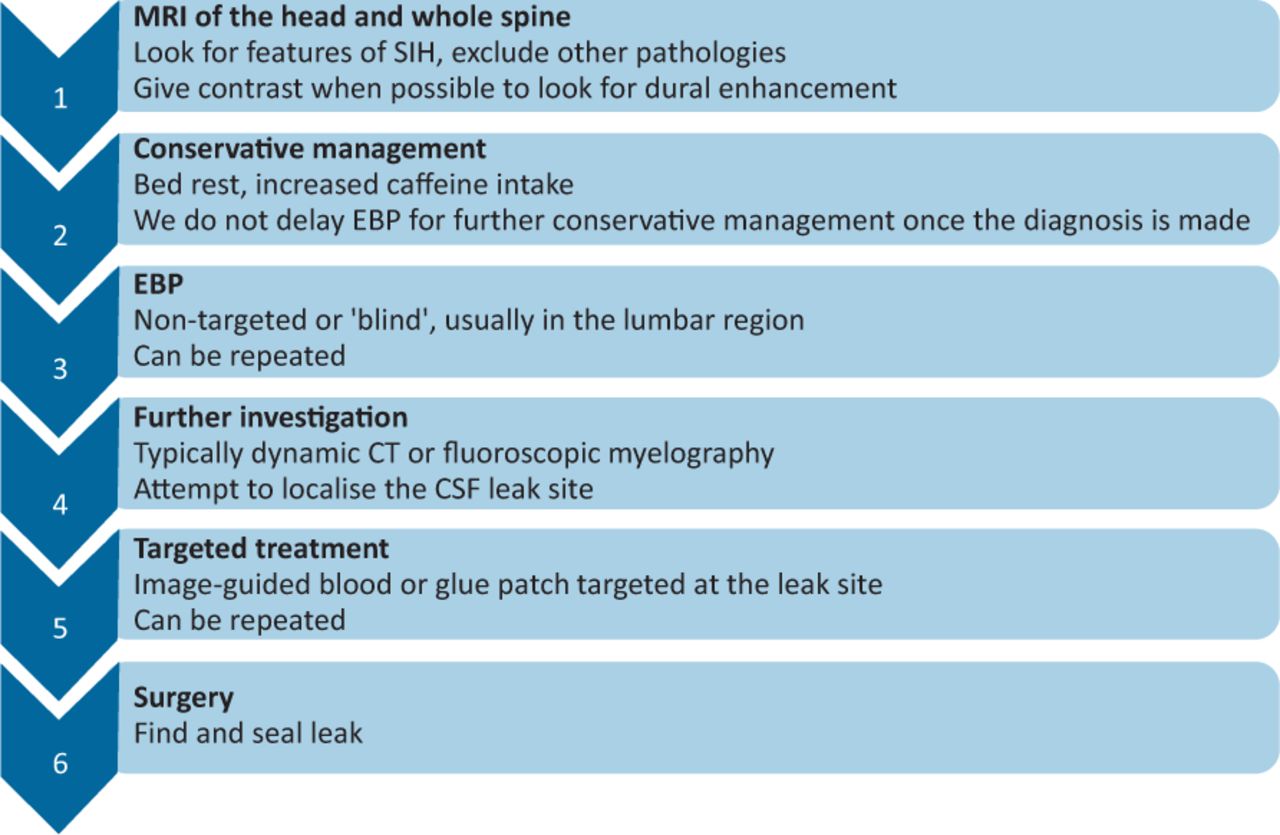
Discussion: The etiology of the left lateral rectus palsy and headaches in this patient with a history of multiple epidural anesthesia procedures, is most likely due to spontaneous intracranial hypotension. Intracranial hypotension is often caused by a CSF leak which can be associated with trauma or can occur spontaneously after sudden movements. The common presentation is orthostatic headaches, worsening with sitting up or standing and improving with laying down. Typically associated with intracranial hypertension rather than hypotension, abducens palsy is the most common cranial nerve palsy in intracranial hypotension. MRI head imaging can be helpful in diagnosing intracranial hypotension with dural thickening and enhancement potentially suggestive of hypotension. While spinal MRIs for our patient were negative for CSF leak, other imaging studies such as CT/MR myelography are generally more effective at identifying a leak and may be used instead.While most cases of intracranial hypotension due to suspected CSF leaks resolve with conservative measures, CSF blood patches are used when symptoms persist and often result in near-immediate improvement in symptoms.
Conclusions: While spontaneous intracranial hypotension is a rare cause of lateral rectus palsy, it should be considered. Although MRI head and spine are usually the first-line imaging modalities, other imaging studies such as CT/MR myelography are generally more effective at identifying a leak. Additionally, it is important to note that blood patches may be acceptable for Jehovah’s Witness patients and have been reported to be used in several such patients.