Background: It is common for Inter-Intensive Care Unit (ICU) transfers between hospitals to take place to provide a patient with a higher level of care to improve clinical outcomes. The decision to transfer ICU patients is not standardized and leads to a wide variability in transfer practice patterns. This may lead to higher cost, burden for family, and increased patient morbidity without the intended clinical benefit. The purpose of this study is to evaluate patterns of suboptimal inter-ICU transfers including those patients who are defined as i) futile transfer (die or transition to comfort measures within 48 hours) or ii) low-value transfer (discharged alive from the receiving hospital within 48 hours).
Methods: We performed a retrospective study assessing patients (age >18 years) who were transferred to various ICUs of a large tertiary care hospital between January 2014 to December 2017 to evaluate our main primary outcomes of futile and low-value transfers. To quantify the hospital-level variation in each outcome, random-slope multilevel logistic regression models with transfers nested within hospitals were utilized. After adjusting for patient characteristics, the median odds ratio (MOR) for transfer was calculated as a measure of variation between hospitals not explained by individual characteristics in the model.
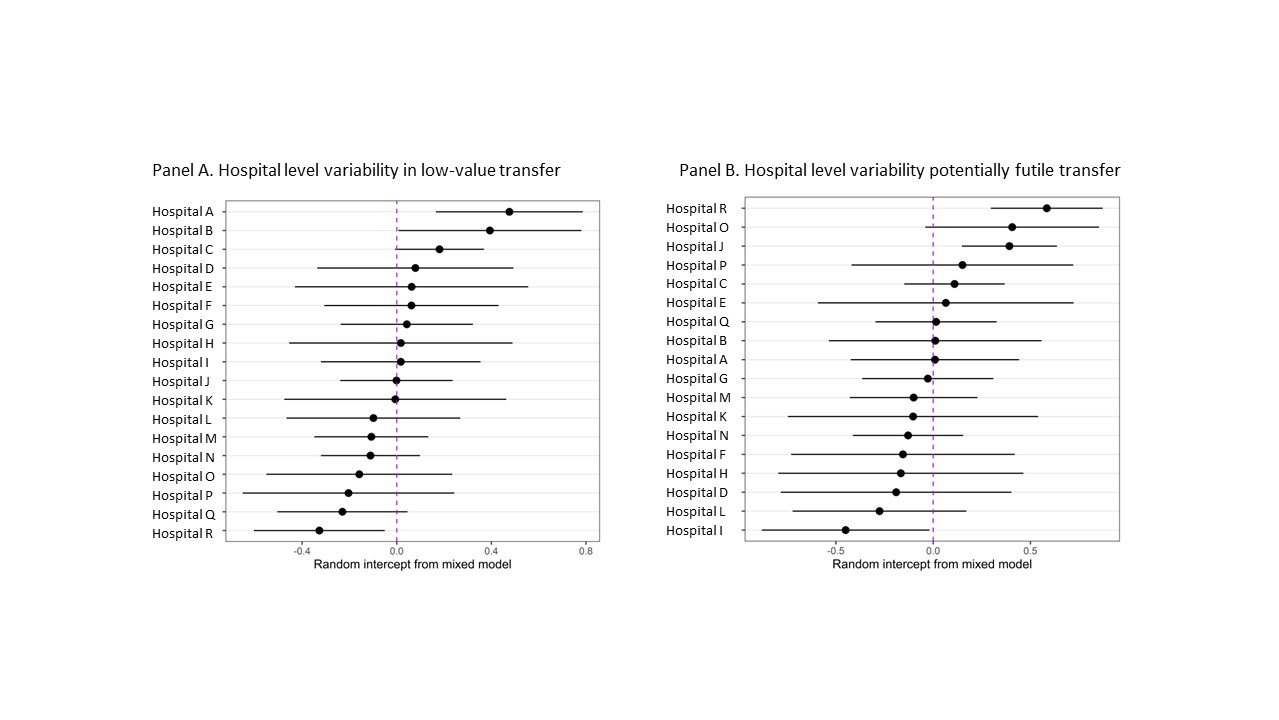
Results: 5,769 patients who were accepted in transfer to the tertiary care hospital from 18 other health system hospitals across North and South Carolina were included. The proportion of patients experiencing potentially futile transfers and low-value transfers was 0-11% and 9-22%, respectively. After adjustment for age, Charlson comorbidity index, and SOFA score, the MORs for potentially futile transfers and low-value transfer were 1.34 [CI: 1.20-1.84] and 1.29 [CI: 1.21–1.38,], respectively. Caterpillar plots demonstrating Hospital-Level Variability in low value transfers (Figure 1, Panel A) and potentially futile transfers (Figure 1, Panel B) are shown.
Conclusions: Transferring ICU patients between hospitals is a common event with approximately 50,000 inter-ICU transfers occurring annually in the United States. Despite its frequency and purported benefit, little standardization exists to guide when to transfer patients, resulting in wide variability in transfer practice patterns and outcomes. Given the high cost and known risks associated with the transfer process, we aimed to understand hospital-level variations in transfer practice patterns. Our study supports that there are significant hospital-level variations in low-value and futile inter-ICU patient transfers. Further work is needed to improve standardization of inter-ICU transfers and understand what patient phenotype and clinical scenario is appropriate.