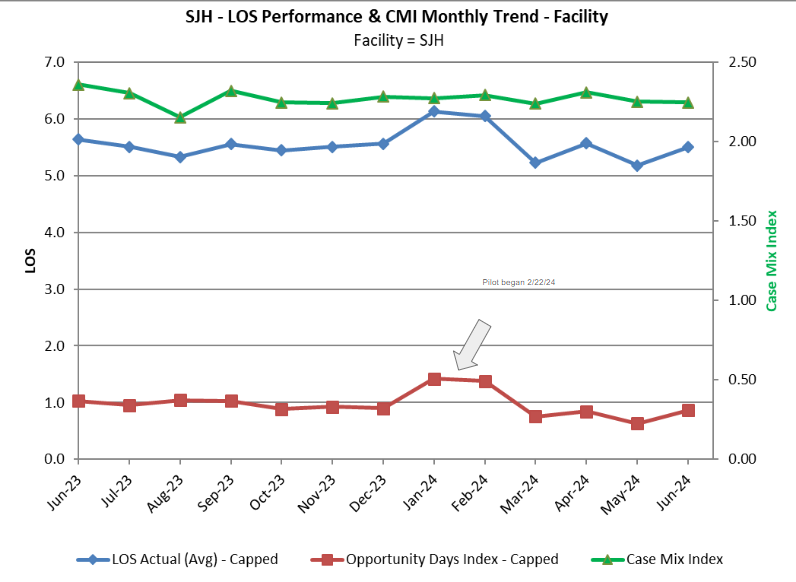
Background: A process problem with our MDR process was identified which had exhausted conventional unit-based approaches to improvement. We researched new processes and brainstormed on an “outside the box” approach to the Case Management model and MDR Daily Meetings. The new approach involved a dramatic Hospital-wide change of structure, associated with integration of multiple service groups. The result was a new CM model/MDR system that has shown improved LOS, collaboration and communication, patient flow and care, along with true partnerships within the care team.
Purpose: The purpose was to re-structure a broken CM/MDR process in an effort to improve patient care and LOS.
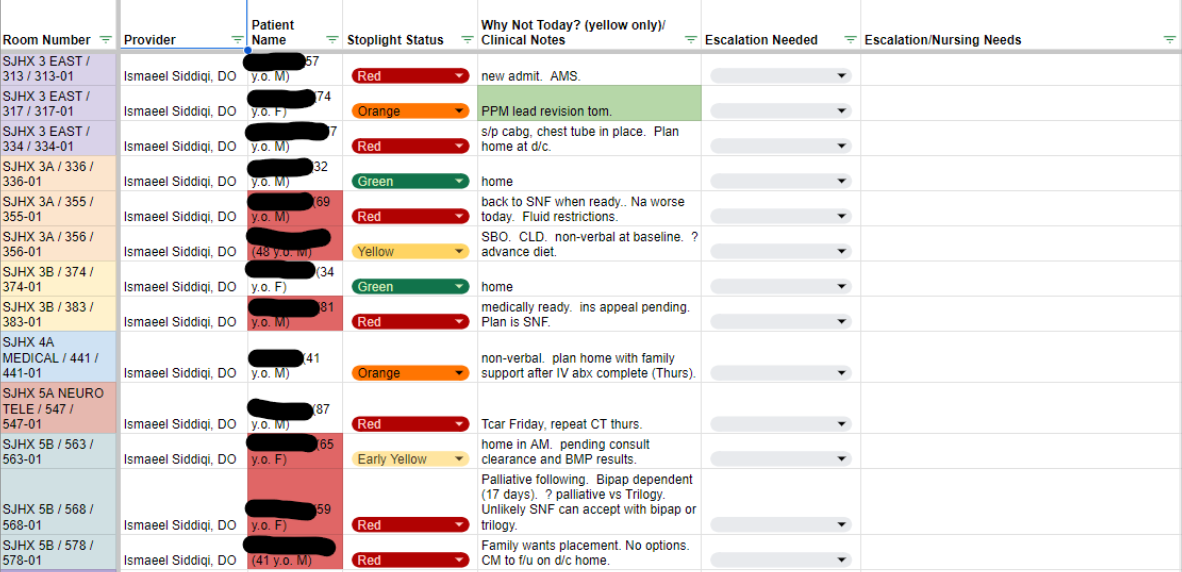
Description: The CM staffing model was changed from a geographic model to a CM/Provider Team model. Each team has a pod of patients which are discussed everyday at MDRs. The CM/Provider team discuss their pod of patients in total every morning and develop a plan of care. This provides Case Management continuity day to day for patients, stronger team partnerships, reduction of texts/calls/chats and duplicated workflow. The MDR meeting was restructured as a rapid case discussion – similar to “speed dating”, members in person and on Zoom, with escalations of barriers to care and flow identified and put on a Global Tracking Sheet and distributed to the team members who can resolve the problems. Members of Nursing, Surgical services, CDI, Physical Therapy, PICC line team are all present with the CM, Provider and Physician Advisor to discuss EVERY patient in the hospital. A system to identify expected discharge was also set up called the “Stoplight” system. A scribe inputs the data into the MDR Global Tracker and this is distributed hospital-wide for all care team members to use as appropriate. Escalations are required to be addressed by early afternoon and resolutions chatted to the provider. Nursing and care team member use the tracking tool to streamline discharges/anticipated discharges and facilitate patient flow and throughput.
Conclusions: We have achieved more collaboration amongst team services, been able to identify barriers and resolve them more quickly, improve LOS and reduce opportunity days significantly, identify unnecessary procedures that can then be shifted to the outpatient setting thus reducing denials, and more proactive discharge planning. Overall, the process change has empowered the Provider, bedside Nurse, and CM with the most information about their patients, which can then be shared with patients and their families thus improving patient satisfaction.