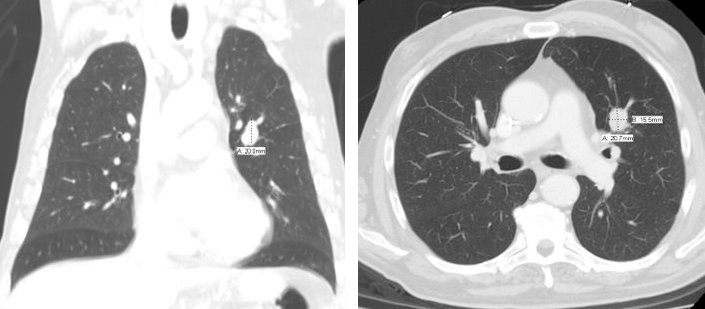
Case Presentation: A 69 year old man with history of Stage IV Mantle cell lymphoma on maintenance Rituximab presented to the emergency department with acute confusion and expressive aphasia. Patient was at his behavioral and functional baseline prior to this episode and there had not been any recent illnesses, medication changes or inciting events. Initial computed tomography (CT) scan of the head did not reveal any acute intracranial hemorrhage or infarction and therefore he was treated with tissue plasminogen activator (TPA). Repeat imaging with head CT and brain magnetic resonance imaging (MRI) did not reveal any intracranial pathology. While his aphasia improved, he developed anterograde amnesia with associated behavioral changes and irritability, and labs revealed rapidly progressive cytopenias. A CT of the chest, abdomen and pelvis was obtained given concern for recurrent Mantle cell lymphoma and it revealed interval increase in size of supraclavicular and mediastinal lymphadenopathy, with a new 2 cm solid nodule within the central left lingula. Cerebrospinal fluid analysis was only remarkable for mildly elevated protein and bone marrow biopsy resulted with metastatic small cell pulmonary carcinoma. Patient was started on intravenous immunoglobulin therapy and on chemotherapy with Carboplatin and Etoposide.
Discussion: Limbic encephalitis is a type of paraneoplastic neurological syndrome (PNS) characterized by short-term memory impairments, personality changes and an acute confusional state. It is an autoimmune response and has been reported in patients with small cell lung cancer. While expressive aphasia has been described in the literature in cases of limbic encephalitis, it rarely is the initial clinical finding. Due to its complex pathophysiology and delayed recognition, curative treatment is difficult to obtain. In addition, there are no randomized controlled trials to guide therapies. In our patient, prior history of lymphoma and immunosuppressive treatment with Rituximab led to a high clinical index of suspicion for infection or recurrent malignancy, but a negative infectious work up and discovery of new primary malignant lesion led to the diagnosis of a PNS. It is imperative to have a high index of suspicion in patients with risk factors who develop acute neurological changes.
Conclusions: Since the presentation of limbic encephalitis is variable, it can lead to a missed diagnosis and delayed treatment. Recognizing a paraneoplastic neurological disorder such as limbic encephalitis as the initial clinical sign of a new malignancy can allow for an earlier therapeutic approach.